Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer




Discovery to Clinic

Outcomes, Quality and Healthcare Performance

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers
Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers
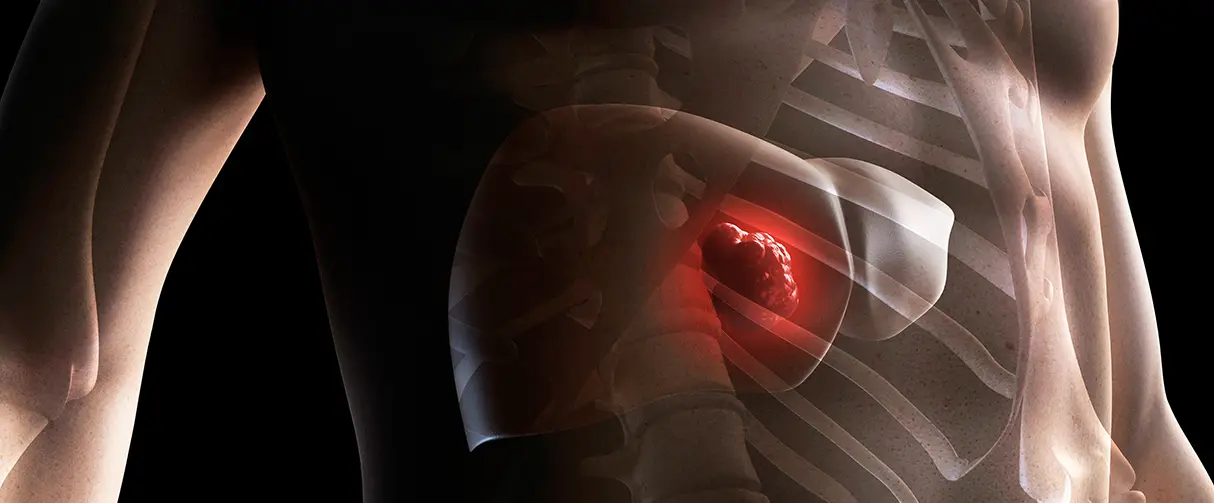
The liver’s legendary ability to regenerate is wonderfully highlighted in the Greek mythology of Prometheus, whose eternal punishment relied on the liver to regrow overnight only to be consumed by Zeus’ eagle the next day. Despite the liver’s prowess at self-renewal, certain cancers can infiltrate the liver enough to prohibit surgical resection. In these cases, transplant oncology offers patients a path toward better disease management, improved health outcomes and a potential cure.

Maen Abdelrahim, MD, PhD
In a review published in the journal Cancers, Maen Abdelrahim, MD, PhD, BPharm, Associate Professor of Medicine in Oncology and his collaborators have presented an overview of the evolution of transplant oncology as a treatment for certain liver cancers that cannot be surgically removed. Further, the authors have discussed the feasibility of neoadjuvant treatments before transplantation and suggest post-transplantation disease surveillance methods to optimize patient care.
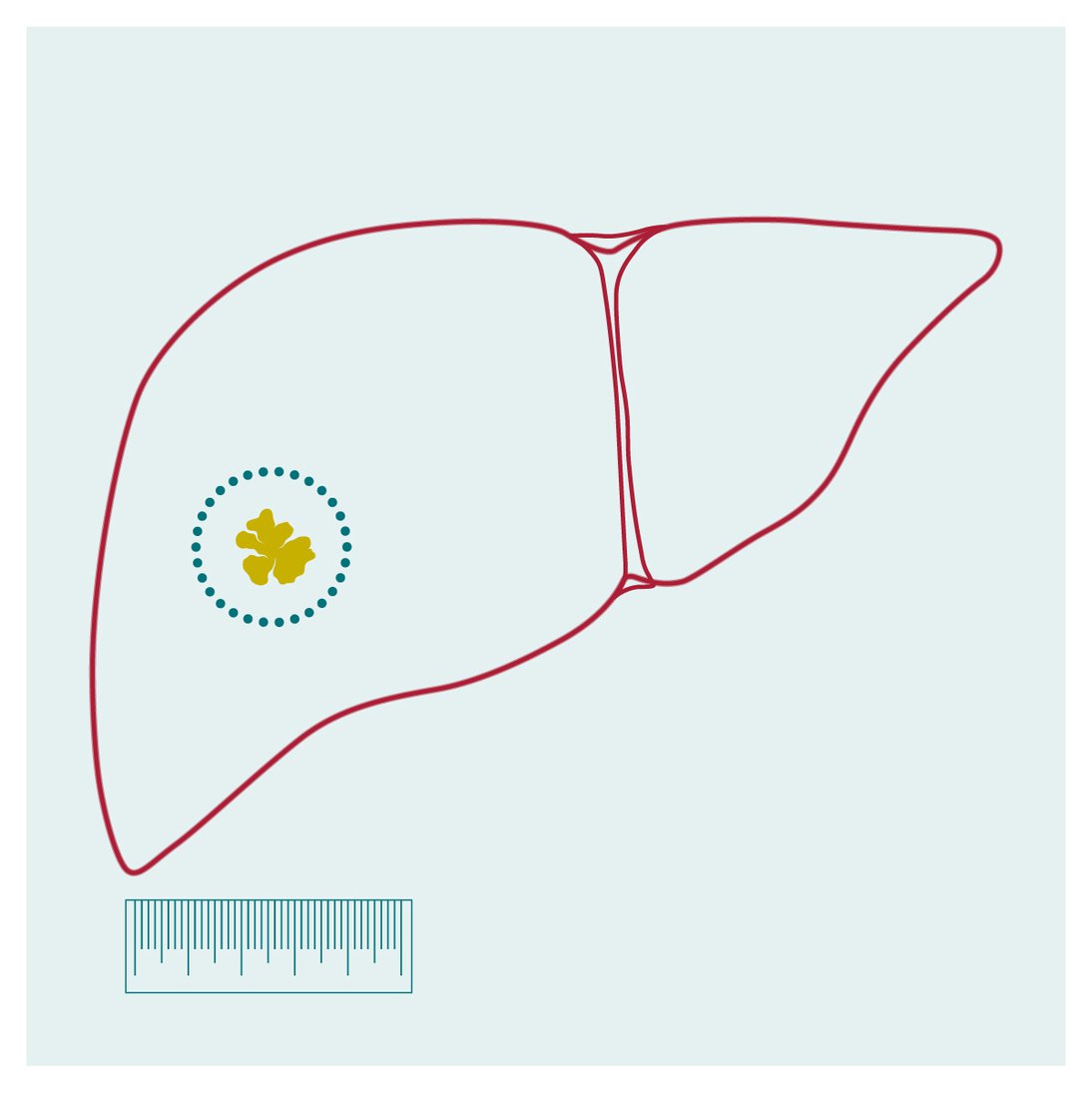
According to the American Institute for Cancer Research, liver cancer is the sixth most common form of cancer worldwide, with a survival rate of around 20%. The most frequently encountered form of liver cancer is hepatocellular carcinoma, which is often observed in people with cirrhosis or chronic liver disease. However, cancers inside and outside the liver are also associated with cholangiocarcinoma and the metastatic progression of neuroendocrine and colorectal cancers.
Patients with liver cancer can be on long-term chemotherapy, which profoundly compromises their quality of life. Hence, when possible, cancerous tissue is surgically removed to mitigate the dependence on drug therapies. But in some instances, the authors explained, the liver is heavily scarred or has widespread cancer, making surgical resection extremely challenging. In these circumstances, liver transplantation is a line of treatment that holds promise to dramatically improve patient survival.
“Unlike for other solid organ transplants where the history of active cancer is considered as a contraindication for transplantation, liver malignancy is one of those special instances where transplantation is a viable treatment option,” said Abdelrahim.
Milan Criteria
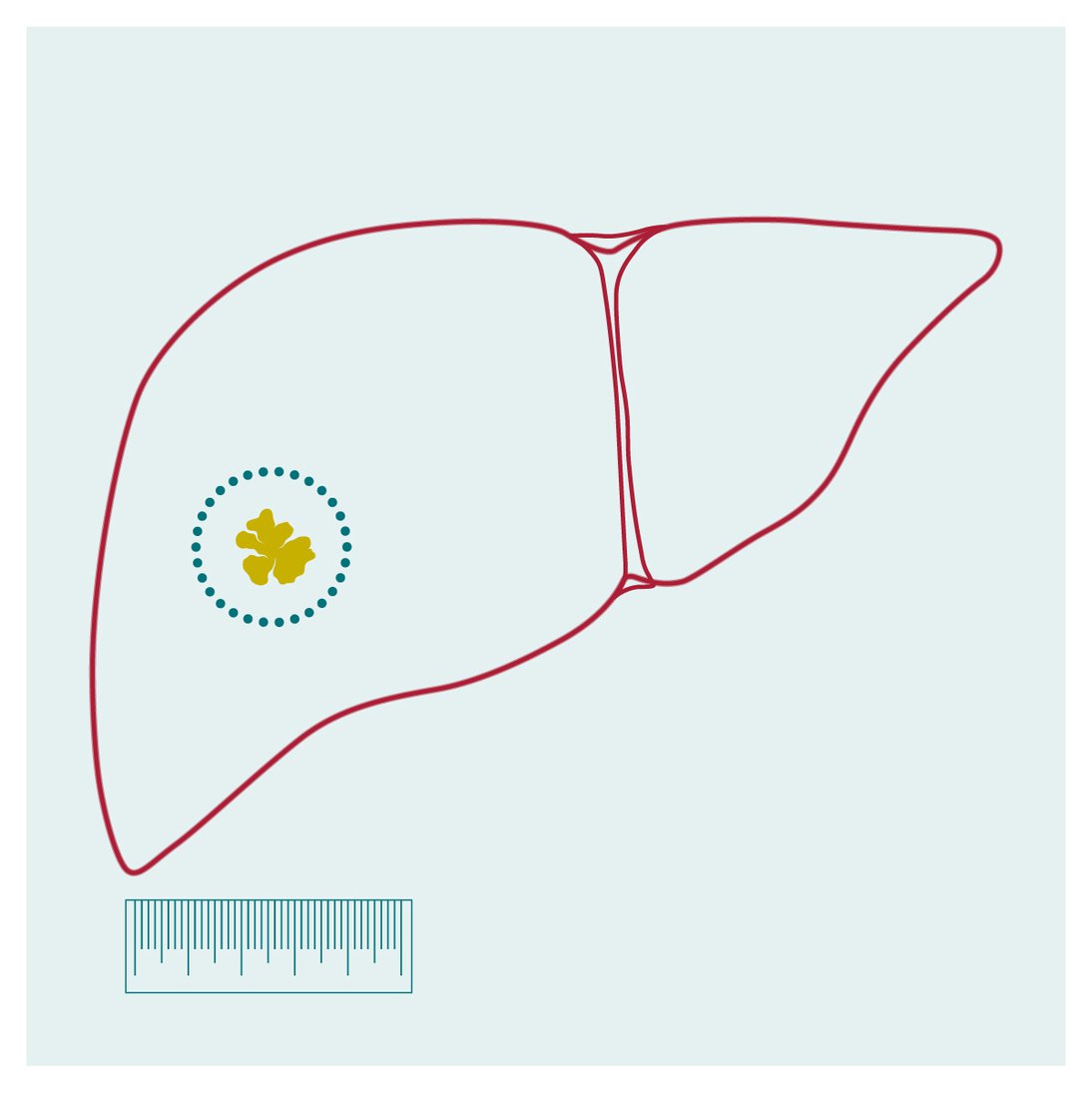
1. Single lesion ≤ 5 cm
Multiple (but within three) lesions ≤ 3 cm
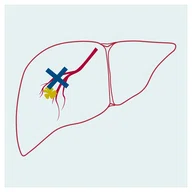
2. No vascular invasion
3. No metastasis
Milan Criteria
1. Single lesion ≤ 5 cm
Multiple (but within three) lesions ≤ 3 cm
2. No vascular invasion
3. No metastasis
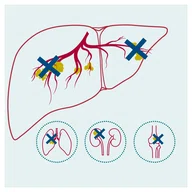
The criteria required to screen hepatocellular carcinoma patients eligible for liver transplants were first laid by Italian physicians in 1996, and these have been dubbed the Milan criteria. This selection protocol requires the tumor diameter for single lesions to be less than or equal to 5 cm, and less than or equal to 3 cm for multiple but within three lesions. In addition, the cancer must have no vascular invasion or metastasis. According to the authors, liver transplants on these patients boost the five-year survival rate to 80%-85%.
However, over the years, the Milan criteria have been expanded to include bigger liver cancers and other unresectable liver malignancies resulting from bile duct and metastatic cancers. In some cases, patients may receive bridge treatments, including chemo and immunotherapy, to downsize liver cancer to meet the Milan criteria for transplantation.
As proof of concept for neoadjuvant bridging therapy, a collaborative effort between the Houston Methodist’s J.C. Walter Jr. Liver Transplant Center and the Dr. Mary and Ron Neal Cancer Center were the first to report a prospective case series of intrahepatic cholangiocarcinoma patients receiving chemotherapy followed by liver transplantation. These patients had a five-year survival rate comparable to those with hepatocellular carcinoma who received liver transplants.
The authors also discussed the feasibility of minimally invasive postoperative disease surveillance methods, particularly liquid biopsies to monitor the circulating tumor DNA in the bloodstream. This technique, they noted, could facilitate detecting small traces of residual disease after transplantation and propensity of disease recurrence.
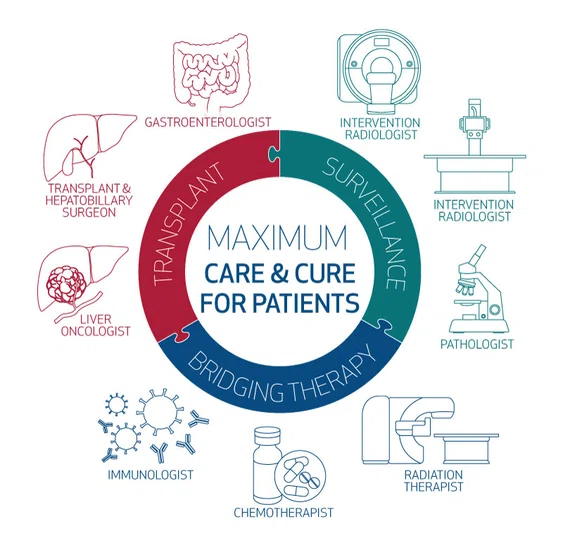
Although a promising treatment for certain unresectable liver tumors, transplant oncology is best suited for hospitals that both specialize in cancer treatment and perform transplantation surgeries at high enough volumes. Further, the field is very interdisciplinary, requiring physicians and scientists belonging to diverse disciplines, including gastroenterology, immunology and radiology, under one umbrella organization. Hence, Abdelrahim noted that Houston Methodist is one of few uniquely poised institutions to be a transplant oncology center of excellence.
“Here, at Houston Methodist, we can, with our expertise, grow and develop the field of transplant oncology, which is a rapidly evolving subspecialty field with very encouraging prospective outcomes,” he said.