Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer


Deepening Insights Into Human Brain Disease

When Aduhelm, a highly anticipated Alzheimer’s drug, was greenlit in June 2021, it sparked renewed hope in pushing back against a debilitating neurodegenerative disease that has crippled more than 6 million of America’s elderly. Unfortunately, Aduhelm was a failure; phase 3 clinical trials indicated inconclusive evidence of the drug’s action, and the therapeutic even posed unforeseen life-threatening side effects. But like many other candidate drugs that have met a similar fate, Aduhelm had outstanding evidence of success in its preclinical research phase.
Each year, several potential therapeutics make their way into the graveyard of drug development failures, costing billions of dollars and prolonging the wait for those patiently waiting for a cure. In fact, more than 30% of drugs that enter phase 2 clinical trials do not progress, and 58% of drugs that pass the phase 2 hurdle eventually fail in phase 3.
The sheer complexity of clinical trial design and implementation certainly contributes to this discouraging statistic. But if aspects of the human disease are not fully recapitulated in model organisms used in preclinical research, these shortcomings could then culminate in the failure of candidate drugs in clinical trials.

Robert Rostomily, MD
This concern has the research community turning toward biorepositories. These institution-maintained libraries contain patient-derived biological samples, clinical reports and other information that provide key access to disease progression in humans. Within the Texas Medical Center, Houston Methodist Biorepository Core maintains a collection of nervous system-related specimens and clinical data from consenting patients within the neural biorepository, or NBRX. In addition, NBRX also contains results from drug response profiling and data gathered from genomic analysis and proteomics.
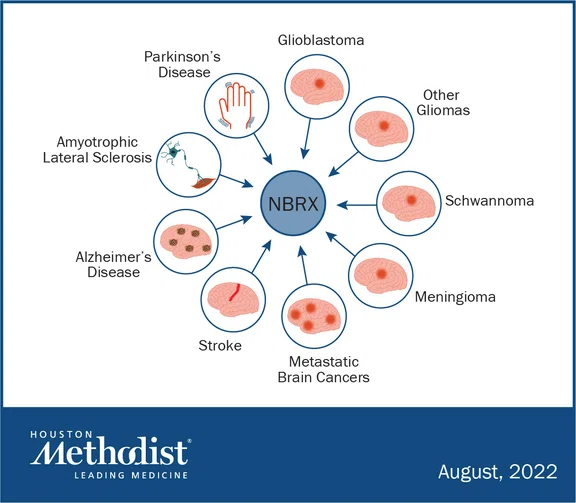

Houston Methodist’s neurorepository, or NBRX, contributes to different areas of clinical and neuroscience research within the Texas Medical Center.
"We now have an important infrastructure that supports studying neuro-oncology, neurodegenerative diseases, strokes and other illnesses that affect the human brain,” said Robert Rostomily, MD, the John S. “Steve” Dunn, Jr. and Dagmar Dunn Pickens Gipe Chair in Brain Tumor Research and principal investigator overseeing the operations of the neurorepository. “Importantly, the access to human-derived samples means we now have realistic platforms that validate to the efficacy of candidate drugs and explore underlying disease mechanisms.”
Currently, a substantial portion of biomedical research is spearheaded by animal research, particularly in mice. Rodents are relatively easy to obtain, breed well in captivity and are born precocious, allowing scientists an opportunity to study developmental processes that are otherwise inaccessible in other species. Nowadays, advanced genetic and molecular tools have transformed rodents into attractive models for research.
But can research in other species stand in for humans? Conventional scientific wisdom tells us that although humans and rodents diverged from a common ancestor around 80 million years ago, certain fundamental aspects of development and physiology are evolutionarily conserved. And certainly, there has been a multitude of discoveries stemming from rodent research in areas spanning immunology, neuroscience, cancer and infectious disease. However, a deeper look often reveals species-specific differences. Neurodegenerative diseases, particularly Alzheimer’s disease, is a glaring example. The illness does not occur naturally in rodents.
“We are realizing more and more that for brain disease, the immune system is a major determinant of responses, whether in DNA damage or inflammation,” said Rostomily. “But the mouse immune system is very different from that in humans, and so it's not surprising that the work on neurodegenerative disease, intracerebral hemorrhages, and strokes have translated very poorly in humans.”
The initiation of NBRX has led to a substantial increase in the collection of neurosurgery patient-derived tissue samples for different types of central nervous system cancers.
Neurorepositories, thus, fill an important gap by providing access to human-derived samples of neurodegenerative disease, cancer, and other brain diseases. At Houston Methodist, patient-derived cancer cells generated from samples stored within NBRX are used to create grafts of primary brain tumors. Then, leveraging the many advantages of rodents, these xenografts are implanted into immunocompromised mice to study cancer progression. Such work has now been extended to investigate metastasized brain tumors and other central nervous system cancers.
“Our database helps people studying meningioma, and we have a group investigating primary central nervous system lymphomas,” said Rostomily. “Samples for these types of studies are very hard to come by, and we have them at our institution.”
In addition to brain cancer research, NBRX contributes to stroke studies at Houston Methodist. When a hemorrhage occurs in the brain, a slew of changes take place in response to the sudden bleed, some of which are protective while others are pathological. The mechanisms underlying the events around a stroke have yet to be fully delineated, and currently, animal models that can accurately capture the condition in humans are lacking. This hurdle, however, could be overcome with tissue collected from hemorrhagic stroke patients and stored in Houston Methodist’s neurorepository.
“We can look at the samples carefully over time to validate observations we have previously made in preclinical models,” said Muralidhar Hegde, PhD, the Everett E. and Randee K. Bernal Centennial Endowed Director of DNA Repair Professor of Neurosurgery. “It's not just the samples but also the insights we gain from clinicians, like Dr. Rostomily, and clinical data that makes our work more relevant to the human condition.”
While an invaluable resource for brain research, the neurorepository takes significant strategic planning. The steps involved are considerable — in- and outpatient consent forms must be collected and samples from the operation theater have to be obtained, processed and stored, all while preserving participant privacy rights. Further, maintaining neurorepository-related spreadsheets, submitting protocols for approval to the Institutional Review Board, and tracking consents are among the other duties that are part of the efforts.
“It’s a very complicated and labor-intensive process,” said Rostomily. “There are a lot of moving parts, and we’re still figuring out ways to get the funding needed to keep this important core facility running smoothly.”
However, with enough support, Rostomily said the neurorepository has the potential to evolve into a more exhaustive and useful database for the Texas Medical Center. In the near future, patient imaging data could be linked with existing genomic and molecular data, and research from different laboratories could be shared and updated on the database. Ultimately, such comprehensive information, he envisioned, may serve as training sets for artificial intelligence that could then integrate all of the data and assist in deciding individualized treatments for patients.
Thus, neurorepositories expand the brain researcher’s toolkit in many ways. By providing access to patient-derived tissue samples, researchers are given a window into understanding disease progression in humans, testing drug efficacy, and improving therapeutics.
“It’s a privilege for us to have a neurorepository at Houston Methodist,” said Gavin Britz, MD, the Candy and Tom Knudson Distinguished Centennial Chair in Neurosurgery and Professor of Neurosurgery. “Patients have given us consent to take their tissue and have entrusted us to make use of it to make the future better by improving lives.”
Samples collected by NBRX are shared across different institutions within the Texas Medical Center to support the collaboration between clinical and research enterprises, thereby advancing basic neuroscience and translational research.
To learn more, visit the Neural Biorepository Core facility.