
President’s Letter
2023 Metrics
Cycle of Translation
Visionary Gifts

Discovery to Clinic

Innovative Education

Translational Luminaries
Introduction
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
Houston Methodist Dr. Mary and Ron Neal Cancer Center
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
COVID-19 Studies
Outcomes Research
Restorative Medicine
Houston Methodist Advances Research into Neural Prosthetics
Noninvasive Spinal Stimulation Works to Restore Movement After Spinal Cord Injury
An Innovative Approach to Treat Even the Most Stubborn-to-Heal Fractures
Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection
Houston Methodist, Rice University, Baylor College of Medicine Design Noninvasive Tech to Help Remove Brain’s Metabolic Waste
Houston Methodist Investigators Nanotechnology Investigators Awarded Prestigious Grants from the Department of Defense
Precision Medicine
Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy
Novel Drug Combination Can Target Triple-Negative Breast Cancer for Treatment
A Houston Methodist and Purdue University Breakthrough May Result in a More Effective Tuberculosis Vaccine
Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease
New Virtual Intensive Care Unit Simultaneously Improves Patient Care and Bed Capacity
result
Introduction
Joint Weill Cornell–Houston Methodist Academic Institute Doctoral Program Welcomes its Inaugural Class
Visionary EnMed Program Soars to New Heights
Neural Control of Organ Degeneration and Regeneration (NeuralCODR) Training Program
Faculty and Research Development
Graduate Medical Education



Science in Service
of
Medicineresult
President's letter
2021 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

From Discovery to Clinic


What is "Discovery to Clinic"?

Restorative Medicine


Houston Methodist Advances Research into Neural Prosthetics

Noninvasive Spinal Stimulation Works to Restore Movement After Spinal Cord Injury

An Innovative Approach to Treat Even the Most Stubborn-to-Heal Fractures

Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection

Houston Methodist, Rice University, Baylor College of Medicine Design Noninvasive Tech to Help Remove Brain’s Metabolic Waste

Houston Methodist Investigators Nanotechnology Investigators Awarded Prestigious Grants from the Department of Defense

Precision Medicine


Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy

New Virtual Intensive Care Unit Simultaneously Improves Patient Care and Bed Capacity

Novel Drug Combination Can Target Triple-Negative Breast Cancer for Treatment

A Houston Methodist and Purdue University Breakthrough May Result in a More Effective Tuberculosis Vaccine

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

Translational Luminaries

Visionary Gifts of Hope
01
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
02
Houston Methodist Dr. Mary and Ron Neal Cancer Center
03
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
04
Houston Methodist Cockrell Center for Advanced Therapeutics
05
Paula and Joseph C. “Rusty” Walter III Translational Research Initiative
06
Jerold B. Katz Academy of Translational Research
07
Infectious Diseases Research Fund
Ushering medical breakthroughs from the lab to the clinic takes many years and millions of dollars. Most promising discoveries are lost in the phase of translation called the “valley of death.” To help bridge the valley and provide our most promising innovations a lifeline, Houston Methodist is drawing on the transformative power of philanthropy.


01
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
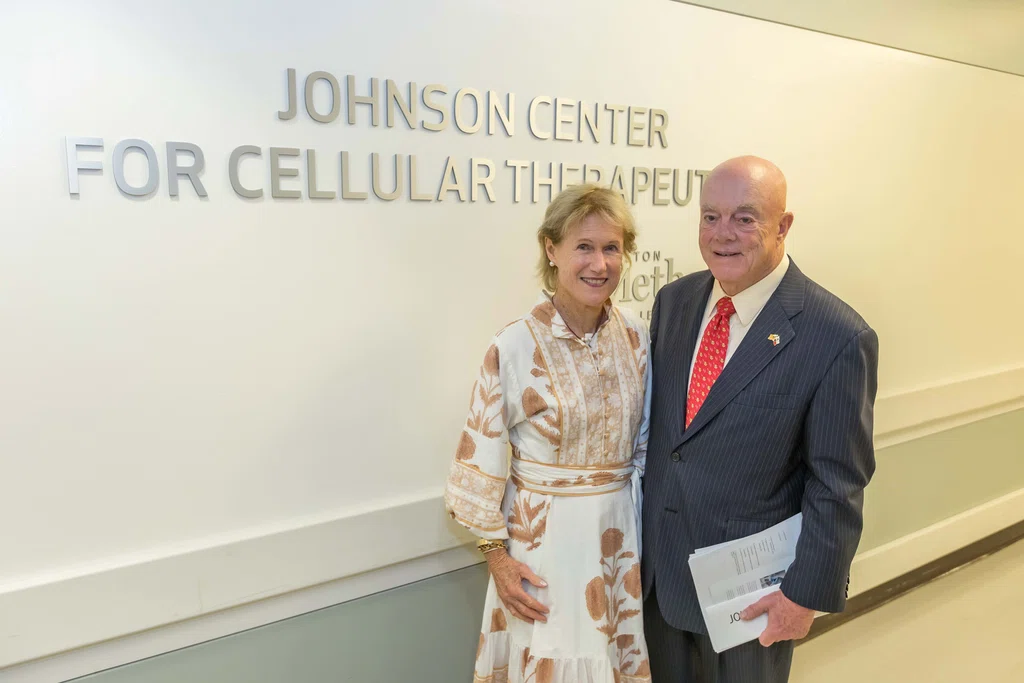
With generous support from Ann and John W. “Johnny” Johnson, Houston Methodist has entered a new era of cellular therapeutics that expands its growing portfolio of immunotherapeutics and RNA therapeutics. Their cornerstone commitment built a research program and production facility at Houston Methodist that allows researchers to design new therapies rapidly and produce experimental therapeutics on-site. The 5,000-square-foot, state-of-the-art, Current Good Manufacturing Practice (cGMP) facility, which opened in 2021, is located in the Houston Methodist Outpatient Center.
Stanley H. Appel, MD, the Peggy and Gary Edwards Distinguished Endowed Chair in ALS Research in the Stanley H. Appel Department of Neurology, will lead a multidisciplinary team of researchers dedicated to expanding cell therapy research at Houston Methodist. His regulatory T cell therapy for amyotrophic lateral sclerosis, or ALS, is demonstrating promising results in slowing disease progression in some patients. Appel’s cell therapy for ALS will be manufactured on-site as part of the cell therapy program at the Johnson Center for Cellular Therapeutics.

Left to right:
- John P. Cooke, MD, PhD, Joseph C. "Rusty" Walter and Carole Walter Looke Presidential Distinguished Chair in Cardiovascular Disease Research
- H. Dirk Sostman, MD, Ernest Cockrell, Jr. Presidential Distinguished Chair at Houston Methodist
- Marc L. Boom, MD, Ella Fondren and Josie Roberts Presidential Distinguished Centennial Chair
- Stanley H. Appel, MD, Peggy and Gary Edwards Distinguished Chair in ALS Research
- Patrick McCulloch, MD, John S. Dunn Chair in Orthopedic Surgery
02
Houston Methodist Dr. Mary and Ron Neal Cancer Center

Houston Methodist received a $25 million philanthropic gift from Dr. Mary and Ron Neal to expand the organization’s cancer center. In recognition of the gift, the Houston Methodist Cancer Center was renamed the Houston Methodist Dr. Mary and Ron Neal Cancer Center.
The gift bolsters the ongoing research led by Jenny C. Chang, MD, Emily Herrmann Presidential Distinguished Chair in Cancer Research and director of the center. Chang’s groundbreaking research has significantly advanced cancer therapy with breakthroughs such as new targeted drugs that alter the tumor immune landscape of triple-negative breast cancer. Mary Neal said that she and her husband wanted to support the incredible work Chang and her associates have been conducting.
The gift also supports three endowed chairs and corresponding research funds as well as ongoing cancer innovation efforts within the Center for Drug Repositioning and Development. Chang also seeks to address neglected populations in the community with the gift and to propel the center’s ongoing research to the national level, toward National Cancer Institute (NCI) designation. The Neals’ gift will elevate the current research and help retain talent to accelerate Houston Methodist’s pursuit of NCI designation.
03
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

The first of its kind in the Texas Medical Center, Houston and the region, the Fondren Inflammation Collaborative is creating a singular destination for patients seeking normalcy and relief from debilitating allergy, immunologic, autoimmune and gastrointestinal conditions. The program was made possible when The Fondren Foundation made a generous $15 million commitment to Houston Methodist. The entire program will be realized in the next decade, helping patients who often get passed between doctors and clinics for months or years in search of a proper diagnosis and treatment plan.
The philanthropic gift strengthens and expands two Houston Methodist programs: the new Immunology Center at Houston Methodist and the Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders. The Fondren Inflammation Collaborative will offer patients one-of-a-kind opportunities to participate in clinical trials focused on innovative treatments and therapies for inflammation-triggered conditions.
Ultimately, the Fondren Inflammation Collaborative will be extended to other disease areas impacted by inflammation, such as the heart, brain, cancer and behavioral health. The gift also will fund four endowed chairs to recruit and retain the best minds in the world while supporting research, education and training efforts.
04
Houston Methodist Cockrell Center for Advanced Therapeutics
Since 2009, The Cockrell Foundation has made generous gifts toward an endowment that supports the Cockrell Center for Advanced Therapeutics (CCAT), which opened its phase 1 clinical trials unit in 2015 and continues to expand today. The knowledgeable staff at the CCAT have the expertise to support all phases of clinical trials, beginning with first-in-human trials. The CCAT brings together world-class medical minds and facilities to study novel therapies for various medical conditions while delivering customized and compassionate care. As part of its deep commitment to developing treatments with ready applicability to human disease, the center aims to make a clinical trial available to every person who needs and wants to participate in one.
The center conducts 24-hour pharmacodynamics and pharmacokinetics evaluations, offers early phase and investigator-initiated trial support services and provides a centralized clinical trials support office. The Clinical Research Phase 1 Unit caters to early phase and proof-of-concept clinical trials as well as precision medicine-focused translational research projects.
As the COVID-19 pandemic took hold across the U.S., the center’s resources and expertise played a critical role in the historic efforts to rapidly activate and conduct clinical trials to evaluate potential therapies for COVID-19. The pandemic also underscored the need for dedicated facilities within the center to support infectious disease clinical trials that require specialized services, equipment, training and protocols. This facility is equipped to facilitate outpatient infectious diseases trials and study-mandated follow-up and data collection after discharge.
Houston Methodist Opens New Facility for Clinical Trials
The Houston Methodist Cockrell Center for Advanced Therapeutics supports all phases of clinical research operations. The center provides more than 7,000 square feet of dedicated space across six locations in the greater Houston area, bringing access to the latest investigational treatment options closer to study participants’ homes or workplaces.
Pandemic Propels Need to Develop a Component of the Cockrell Center for Advanced Therapeutics to Administer Clinical Trials for Infectious Diseases
Houston Methodist is fortunate to find itself in the very good position of having donors who believe in its mission and wish to provide support. One such donor is Reynolds and Reynolds, an automotive retailing company. Through a personal relationship with Ernest D. Cockrell II, Reynolds and Reynolds donated to Houston Methodist, with half of that amount earmarked for outcomes research and the other half for the Reynolds and Reynolds Company Infectious Disease Research Unit; this unit is part of the Cockrell Center for Advanced Therapeutics (CCAT) that is housed in the Houston Methodist Research Institute.
The pandemic heightened the need to develop a component of CCAT that will administer clinical trials for infectious diseases, beginning with COVID-19 patients. These trials require specialized facilities, equipment, training and protocols. This initiative is a component of Houston Methodist’s overall strategy to lead medicine in the prevention and treatment of infectious diseases, which ultimately will lead to the establishment of an Infectious Diseases Center of Excellence.
Beyond COVID-19, Houston Methodist will continue with clinical trials under CCAT for the Dr. Mary and Ron Neal Cancer Center, Center for Outcomes Research, Pathology and Genomic Medicine and several others. The Reynolds and Reynolds Company unit will enable Houston Methodist to conduct clinical research in infectious diseases, which it otherwise would be unable to do, to benefit the Houston community.
Cockrell Center For Advanced Therapeutics
1
Houston Methodist Research Institute
Ccat - Tmc
Clinical Research Phase 1 Unit - Tmc
Reynolds and Reynolds Company Infectious Disease Research Unit
2
Houston Methodist Sugar Land Hospital
3
Houston Methodist West Hospital
4
Houston Methodist Continuing Care Hospital
Highly Infectious Disease Unit Clinical Trials Center
5
Houston Methodist Primary Care Group in Pearland
6
Houston Methodist The Woodlands Hospital
Pinch to zoom image
05
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
When Houston Methodist launched the Translational Research Initiative in 2014, the aim was twofold: provide vital funding to promising new therapies ready to make the transition from research laboratory to clinical use and capitalize on Houston’s bold entrepreneurial spirit to lead the way toward a new model of medical innovation.
The Translational Research Initiative (TRI) provides vital funding for Houston Methodist’s brightest minds to translate new, innovative treatments into bedside-ready therapies and medicines more quickly and at a fraction of the cost of typical innovations. Exceeding expectations, the TRI has enabled Houston Methodist to launch its third phase after securing more than $20 million for translational research projects. The first iteration of TRI, which became known as TRI I when a second initiative was created, began with a philanthropic matching fund established by Paula and Joseph C. “Rusty” Walter III.
The success of TRI I spurred TRI II, which was started through the generosity of the Jerold B. Katz Foundation. The Katz Foundation’s $5 million challenge gift helped raise another $5 million from community visionaries.
Building on the success of TRI I and TRI II, a third initiative was established with another matching challenge gift from Paula and Rusty Walter. The goal of TRI III is to create a $10 million fund much like its predecessors, with one major difference: these funds will focus solely on neurology and translational projects, such as neurosurgery, stroke recovery or Alzheimer’s disease. Beneficiaries of the $10 million fund include Brian Parrish, PharmD, cardiology clinical specialist; Philip Horner, PhD, professor of neurogeneration and scientific director of the Center for Neurogeneration and Gavin Britz, MD, Candy and Tom Knudson Distinguished Centennial Chair in Neurosurgery, director of the Houston Methodist Neurological Institute.
Houston Methodist Walter Tower
ANATOMICALIGNER USES STATE-OF-THE-ART GRAPHICS TO HELP PRESURGICAL PLANNING
Due to the complex nature of the craniofacial skeleton, corrective surgeries require extensive presurgical planning. As a result of the Katz Foundation’s challenge gift, a donation from the Albert and Margaret Alkek Foundation funded the Anatomic Aligner, a free software program, online Surgical Planning for Jaw Deformities Website and eBook that uses information acquired from multiple imaging modalities to simulate jaw surgery. This gift made it possible for Jaime Gateno, MD, DDS, professor and chair of the Department of Oral & Maxillofacial Surgery, and James Xia, MD, PhD, professor of oral maxillofacial surgery, to realize their vision of launching these much needed global resources that can be freely accessed by physicians and patients facing severe facial deformities.
Approved by the U.S. Food and Drug Administration, the AnatomicAligner uses state-of-the-art computer graphics and modeling to help reduce unwanted surgical outcomes and procedures. The website explains how to use the computer aided surgical system to plan delicate and difficult facial reconstructive surgeries to repair facial deformities through the use of 3-D imaging data or computerized tomography to simulate different types of surgery before physically touching the patient.
1
Before surgery, Lindsay’s bone structure was not symmetrical.
2
AnatomicAligner software calculated which adjustments were needed to achieve symmetry.
3
After two extensive surgeries, Lindsay wore braces for several weeks. With newfound confidence, she began her career at a large corporation.
Innovative Magnetic Device Shows Promise for Treating Brain Injury
A noninvasive smartphone-compatible magnetic stimulation cap developed at Houston Methodist is helping patients make a functional recovery following brain injury or dysfunction. Invented by Santosh Helekar, MD, PhD, associate professor of neurosurgery at Houston Methodist, and Henning Voss, PhD, associate professor of physics in radiology at Weill Cornell Medical College, this affordable, portable and wireless technology uses novel transcranial stimulation technology to modulate neural activity in multiple parts of the brain simultaneously.
When Helekar collaborated with David Chiu, MD, the Elizabeth Blanton Wareing Chair in the Eddy Scurlock Stroke Center, to test the device in a phase 2/3a clinical trial involving 30 ischemic stroke survivors with motor impairment, the cap increased neural activity near stroke-injured areas of the brain, inducing a trend toward recovery of motor function. The cap is also being tested for other applications, such as improvement of bladder control in multiple sclerosis.
To date, the cap technology has been granted four patents by the U.S. Patent and Trademark Office, all of which have been licensed to a startup company called Seraya Medical LLC. A larger multicenter stroke trial and submission for regulatory clearance are being planned.
06
Jerold B. Katz Academy of Translational Research
The Jerold B. Katz Academy of Translational Research at Houston Methodist was funded through the Jerold B. Katz Foundation to recruit and retain the world’s most promising transformational researchers in health care. According to Evan H. Katz, one of Jerold B. Katz’s sons and the president of the Jerold B. Katz Foundation, the gift is designed to continually seed innovation and facilitate the discovery of improved treatments and medications. A portion of the gift supports the research efforts of eight investigators, four of whom are currently in place. The fourth of the investigators, Rodney J. Folz, MD, PhD, was announced in 2021.
KATZ INVESTIGATORS
Nestor F. Esnaola, MD, MPH, MBA, FACS
Esnaola is the associate director of cancer control and population science at the Houston Methodist Dr. Mary and Ron Neal Cancer Center and professor of surgery and division head of surgical oncology in the hospital’s Department of Surgery. He works closely with the Dr. Mary and Ron Neal Cancer Center director Jenny C. Chang, MD, Emily Herrmann Presidential Distinguished Chair in Cancer Research, to drive efforts in the areas of cancer prevention, community outreach and engagement, cancer health disparities and population science research. Esnaola is using the Katz Investigator funding to evaluate a patient navigation intervention tool intended to optimize breast cancer care and address outcome disparities in minorities and underserved women. The tool will be tested in a large-scale, community-based, randomized clinical trial.
Khurram Nasir, MD, MPH
Nasir is a professor of cardiology, chief of the Division of Cardiovascular Prevention and Wellness in the Houston Methodist DeBakey Heart & Vascular Center and co-director of the Center for Outcomes Research at Houston Methodist. Nasir is using the Katz Investigator funding to support his efforts to develop a systemwide hospital resource for research in the area of cardiovascular disease prevention. This platform will harness the power of big data, innovative computation paradigms and artificial machine intelligence to integrate clinical and research data of patients with cardiovascular disease. By leveraging dashboards and digital solutions like alert systems and automatic prescriptions, Nasir aims to identify gaps in preventative care among high-risk individuals.
Trisha L. Roy, MD, PhD
Assistant professor of cardiovascular surgery, vascular surgeon-scientist and Katz Investigator at Houston Methodist, Roy is researching advanced imaging options to improve procedural outcomes for peripheral arterial disease. Current imaging techniques fall short at accurately characterizing arterial lesions, which leads to a “one-size-fits-all” approach to treatment. Roy is developing a peripheral arterial magnetic resonance imaging method for evaluating blood vessel blockages that will allow surgeons to precisely tailor surgeries and endovascular procedures to individual patients. By selecting the right treatment for the right patient, Roy hopes to reduce failure rates and make these treatments more successful.
Rodney J. Folz, MD, PhD
Folz, a nationally recognized authority in pulmonary disease, is division chief of pulmonary, critical care and sleep medicine at Houston Methodist. He will use the Katz Investigator funds to further understanding of asthma and chronic obstructive pulmonary disease (COPD), with an eventual focus on asthma-COPD overlap syndrome, including examining bioactive lipids associated with oxidative stress to determine a racial phenotype for older adults with asthma. Folz also will support an ongoing collaboration with investigators at the Texas A&M Institute of Biosciences and Technology to identify mechanism-based sensitive biomarkers of genomic instability, proteomics and immune cell profiling for early diagnosis and disease prevention of COPD.
07
Infectious Diseases Research Fund
As a hospital founded over a century ago to serve a city ravaged by the Spanish flu, Houston Methodist was destined to take a leading role in the COVID-19 response. Like during the hospital’s early days, philanthropic visionaries played a pivotal role in making it possible for Houston Methodist’s front-line workers to provide lifesaving care. When the pandemic erupted in March 2020, three longtime Houston Methodist supporters — Ann and John Bookout III, Diane and David Modesett and the Jerold B. Katz Foundation — created a challenge initiative to support the Houston Methodist Infectious Diseases Research Fund (IDRF): They offered to match gifts dollar for dollar. Through this act of generosity, physician leaders developed innovative COVID-19 therapies and clinical practices, setting the stage for Houston Methodist to lead in the fight against COVID-19 and future disease outbreaks. The challenge goal was reached within two weeks.
Spurred by this overwhelming response, the Modesetts, Freeport LNG and the Ting Tsung and Wei Fong Chao Foundation established a second challenge initiative to meet their goal in even less time than the first challenge. Since then, with these research dollars in place, the team rapidly translated their scientific findings into better treatments that benefited patients and impacted the disease response nationwide. Houston Methodist became the first academic medical center in the U.S. to infuse critically ill COVID-19 patients with plasma donated by recovered patients. The generous support of its donors enabled Eric Salazar, MD, adjunct associate professor of Pathology and Genomic Medicine PhD, and James M. Musser, MD, PhD, Fondren Presidential Distinguished Chair in the Houston Methodist Research Institute and professor and chair of the Department of Pathology and Genomic Medicine, to conduct a study titled, “Treatment of COVID-19 Patients with Convalescent Plasma Reveals a Signal of Significantly Decreased Mortality.” The study demonstrated that transfusion of plasma containing high levels of anti-SARS-2 antibodies within 72 hours after hospitalization is the most effective way to provide this therapy to critically ill COVID-19 patients.
The Infectious Diseases Research Fund has led to establishment of the Center for Infectious Diseases at Houston Methodist.
According to Musser, “We will next create a Center of Excellence in Infectious Diseases, which will serve as a comprehensive hub for infectious disease diagnosis, treatment, research, education and public outreach. It is because of you that we have gotten so far so fast. It is with you that we will step into the future exceptionally well prepared to attack the next infectious diseases outbreaks and pandemics because history tells us they will occur.”














