
President’s Letter
2023 Metrics
Cycle of Translation
Visionary Gifts

Discovery to Clinic

Innovative Education

Translational Luminaries
Introduction
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
Houston Methodist Dr. Mary and Ron Neal Cancer Center
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
COVID-19 Studies
Outcomes Research
Restorative Medicine
Houston Methodist Advances Research into Neural Prosthetics
Noninvasive Spinal Stimulation Works to Restore Movement After Spinal Cord Injury
An Innovative Approach to Treat Even the Most Stubborn-to-Heal Fractures
Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection
Houston Methodist, Rice University, Baylor College of Medicine Design Noninvasive Tech to Help Remove Brain’s Metabolic Waste
Houston Methodist Investigators Nanotechnology Investigators Awarded Prestigious Grants from the Department of Defense
Precision Medicine
Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy
Novel Drug Combination Can Target Triple-Negative Breast Cancer for Treatment
A Houston Methodist and Purdue University Breakthrough May Result in a More Effective Tuberculosis Vaccine
Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease
New Virtual Intensive Care Unit Simultaneously Improves Patient Care and Bed Capacity
result
Introduction
Joint Weill Cornell–Houston Methodist Academic Institute Doctoral Program Welcomes its Inaugural Class
Visionary EnMed Program Soars to New Heights
Neural Control of Organ Degeneration and Regeneration (NeuralCODR) Training Program
Faculty and Research Development
Graduate Medical Education



Science in Service
of
Medicineresult
President's letter
2021 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

From Discovery to Clinic


What is "Discovery to Clinic"?

Restorative Medicine


Houston Methodist Advances Research into Neural Prosthetics

Noninvasive Spinal Stimulation Works to Restore Movement After Spinal Cord Injury

An Innovative Approach to Treat Even the Most Stubborn-to-Heal Fractures

Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection

Houston Methodist, Rice University, Baylor College of Medicine Design Noninvasive Tech to Help Remove Brain’s Metabolic Waste

Houston Methodist Investigators Nanotechnology Investigators Awarded Prestigious Grants from the Department of Defense

Precision Medicine


Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy

New Virtual Intensive Care Unit Simultaneously Improves Patient Care and Bed Capacity

Novel Drug Combination Can Target Triple-Negative Breast Cancer for Treatment

A Houston Methodist and Purdue University Breakthrough May Result in a More Effective Tuberculosis Vaccine

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

Translational Luminaries




Discovery to Clinic
COVID-19 Studies

Houston Methodist Researchers Step Up and Face the Challenges of COVID-19 Virus

Houston Methodist Researchers Step Up and Face the Challenges of COVID-19 Virus

When the COVID-19 pandemic arrived, the scientific and medical communities had limited information about how to treat people infected with the novel virus. Even so, Houston Methodist was well positioned to meet the urgent need for diagnostics, treatments, vaccines and critical medical technologies.
Throughout the pandemic, our research groups continued their studies without interruption. In fact, Houston Methodist researchers submitted 32 more funding proposals during 2020 than they did the previous year. Many investigators quickly pivoted their research focus to COVID-19-related challenges by participating in more than 50 preclinical studies and clinical trials that resulted in more than 170 COVID-19-related published journal articles and 16,000 media placements.
01
At One-year Anniversary of COVID-19 Vaccines, CURATOR Data Still Produces Vital Contributions
Share this story
Farhaan S. Vahidy, PhD, MBBS, MPH
The Moderna and Pfizer COVID-19 vaccines were released in December 2020, completely altering the unfolding narrative of COVID-19's impact on the world. March 2020 became a month of profound change for most of the United States as the emergent virus took a firm hold on the country. While most of the health care world was scrambling to learn how to treat this novel virus, the Center for Outcomes Research at Houston Methodist was in a unique position.
Farhaan S. Vahidy, PhD, MBBS, MPH, the Coneway Family Centennial Endowed Directorship in Quality and director of outcomes at the Center for Outcomes Research, arrived at Houston Methodist in January 2020. He started assessing systems across Houston Methodist’s academic medical center and seven community hospitals to establish the infrastructure for a learning health care system (LHS). The LHS would merge evidence-based medicine and practice-based evidence, relying on clinicians and researchers to provide and use big data through a continual process that achieves ever-improving patient care in a real-time health care setting.
While the pandemic put the initial comprehensive vision of the LHS on hold, the mechanisms were in place for the creation of the COVID-19 Surveillance and Outcome Registry, or CURATOR. Vahidy led a cross-departmental team to create a database designed to digitize COVID-19-related health information, support multiple observational COVID-19 projects and share validated phenotypic data. CURATOR capitalizes on several systemwide data sources, including electronic health records, virtual ICU, CareSense (mobile-first digital platform designed to guide patients through their care) and imaging data warehouses.
As an academic medical center, Houston Methodist had the skills, expertise and leadership needed to fight the virus. But it’s also a complex health care system and, like many others, has information silos, said Vahidy. CURATOR aims to tear down those silos. The database was organized under the Retrospective Research Task Force (RRTF). Dirk Sostman, MD, Houston Methodist Chief Academic Officer, established the RRTF at the beginning of the pandemic, giving it full institutional support and autonomy to operationalize a bioinformatics pipeline to help prioritize and facilitate COVID-19 research. The RRTF collaborated with the hospital’s Institutional Review Board, which approved the CURATOR research database to address operational needs, outcomes research and institutional reporting.
“Houston Methodist’s big data infrastructure and data engineering teams proved to be highly agile and adaptable, which made it possible to establish a robust COVID-19 analytics pipeline in literally weeks. The ability to generate and implement scientific evidence was phenomenal. We consider ourselves battle tested and have confidence in our capacity to respond quickly in the midst of a global pandemic, with the majority of the teams working remotely,” said Vahidy. "The database draws on information collected from every individual tested for COVID-19 at Houston Methodist, as well as any information we have about that patient from before the pandemic began and/or after being tested."
CURATOR can sort these individuals first by those who test positive and those who test negative. Categories can then be further subclassified by whether they were hospitalized, due to COVID-19 or another health condition, and whether they had encounters with Houston Methodist prior to the pandemic. "Looking at the overall picture of a patient's health, even components unrelated to COVID-19, provides clinicians and researchers with very rich longitudinal data. This becomes an important control and is critical for elevating hypothesis generation and testing," said Vahidy.
Data gleaned from CURATOR already has made an impact. Outcomes show the team has been successful at sustaining lower mortality rates; in fact, national comparisons place the Houston Methodist critical care team’s success rates among the highest in the nation. Evidence-based comparisons between Houston’s first COVID-19 surge, from March 13 to May 15, 2020, and the resurgence that occurred May 15 to July 7, 2020, offered real-time data about patients’ socio-demographics, diagnoses, treatments, suitability for enrollment in clinical trials and outcomes. The data highlights disparities within populations. Early on, CURATOR showed a disparity along socioeconomic and racial lines, with higher rates of infection among minorities. Data from the second surge showed a demographic shift toward a younger, predominantly Hispanic and lower socioeconomic patient population with an overall lower comorbidity burden, ICU admission rate and in-hospital mortality. This information is invaluable when it comes to community outreach and provides researchers with innumerable hypotheses to explore.
While COVID-19 information still is being loaded into the database, the CURATOR team is following the efficacy of the COVID-19 vaccines and long-term effects of the virus, but it has also turned its attention to other areas it believes CURATOR can support. The question has become: Since only around 13% to 14% of the population has been infected by the virus, how has it impacted the other 85%? Researchers also have started using CURATOR’s data to look at how members of the older population, who have not been infected, have been affected since the pandemic began. Researchers have looked at vulnerable, older populations, especially those with cognitive impairment or even mild cognitive impairment, not necessarily Alzheimer’s disease or dementia.
The team is interested in learning what the regular care of all populations has been since the disruption of primary care to determine any potential disparities in regular care since the pandemic. Early numbers indicate primary care visits decreased during the pandemic, so routine health care was not achieved. The team presented their recent findings at the Texas Alzheimer's Research Council Symposium in January 2022 in Austin. They have also submitted a paper to the Alzheimer's & Dementia journal that's currently under review. The team believes it has demonstrated, through the CURATOR data, that this susceptible and vulnerable population has been disproportionately affected due to the loss of primary care and access to emergency care. The team also is now beginning to evaluate not just acute care but also chronic disease management. Hypertensive and diabetic patients and those with high cholesterol also need primary care for secondary prevention, and this care also has been disrupted. These hypotheses can directly be studied from CURATOR.
“From a data/bioinformatics pipeline development standpoint, what we have been able to do with CURATOR and COVID data is applicable across any clinical domain. For instance, as a system we need to create cancer, cardiovascular or cerebrovascular disease registries. We have developed a framework on how to maximize the clinical data that we have and give it a structure and put it to use so that we can rapidly gain insights,” said Vahidy.
"I think Houston Methodist is unique in that we have an institutional understanding and commitment at all levels of leadership, starting from the very top, of the importance of creating value from data. If that piece is missing in an organization, the technical advancement and implementation usually does not happen well. We not only have to maintain this, but we also need to grow – both in depth to enhance our bioinformatics pipeline and in breadth to expand cross-institutionally. Therefore, the organizational behavioral part is extremely important.”
“Our commitment to our patients, to their families, to our communities and to the larger scientific audience demands that we always question what we do. We need to be in a constant state of analysis and understanding the consequences of our practices, our behaviors and our policies, and be ready to adapt and change when the evidence presents itself. The stakes are high, we need to be making informed, evidence-based decisions and everyone needs to do their part in creating a health care system that has a culture of constant learning. To me, that's the important piece. Even beyond COVID, we need to tune our thought process and be ready to modify behaviors and practices. That's just how we operate – we make data-driven and evidence-based decisions and continuously evaluate ourselves to do what is best for our patients and their families, with the goal of constantly improving patient outcomes and experience.”
Farhaan S. Vahidy, PhD, MBBS, MPH
Coneway Family Centennial Endowed Directorship in Quality and director of outcomes, Center for Outcomes Research
02
Research
Houston Methodist Study Reveals Masks and Distancing Decrease Transmission of Seasonal Infections

A Houston Methodist study showed a rapid return of seasonal respiratory viruses after COVID-19 restrictions were relaxed in Texas, demonstrating the effectiveness of masking, distancing and other precautionary measures at stopping the spread of many respiratory illnesses, not just COVID-19.
This rise in non-COVID respiratory viruses to pre-pandemic levels came on the heels of Texas ending its mask mandate in early March 2021 and lifting restrictions on businesses, which could resume operating at 100% capacity. Further contributing to the spike in cases were the updated COVID-19 guidelines from the Centers for Disease Control and Prevention in mid-May that caught many by surprise, giving the fully vaccinated license to resume activities without masks or distancing, though two months later masking was reinstated for everyone when the Delta surge took hold in July.
The findings made by S. Wesley Long, MD, PhD, medical director of diagnostic microbiology at Houston Methodist, and his team, titled “The reemergence of seasonal respiratory viruses in Houston, Texas, after relaxing COVID-19 restrictions,” appeared in the Fall 2021 issue of Microbiology Spectrum, a peer-reviewed scientific journal published by the American Society for Microbiology. This relaxation of mask mandates and social distancing and decrease in vaccination rates ultimately led to the fourth surge seen in many parts of the country this past summer and proved to be the worst surge of the pandemic to date.
When Long and his team noticed a cluster of seasonal non-COVID coronavirus infections diagnosed at Houston Methodist in the spring of 2021, they pulled the data for the respiratory pathogens in Houston. They found while rhinovirus and enterovirus infections started to rebound in the fall of 2020 after the capacity limits for bars and restaurants were relaxed in Texas, the seasonal non-COVID coronaviruses, parainfluenza and respiratory syncytial virus (RSV) were showing robust increases in cases during the four months after the mask, distancing and occupancy mandates were rolled back. The study’s series of histograms illustrates the striking ebb and flow of non-COVID respiratory virus diagnoses in Houston through each stage of precautionary measures being enacted and relaxed. The research team observed a month-over-month increase in parainfluenza and seasonal coronaviruses. Cases of RSV increased dramatically in the summer months; from April to June 2021, the Houston area saw an increase of more than 200% in RSV cases. Long notes similar increases in RSV were seen elsewhere, notably in Australia, after COVID-19 measures were relaxed there. Since the study, which tracked these viruses through the end of June, the number of RSV cases peaked in July 2021.
Long said his team also saw an increase in rhinovirus and enterovirus in August and September of 2021, but that these common cold viruses declined later that Autumn since that rise in cases was likely related to schools reopening. He said these peaks were out of season, in part due to Texas removing its final COVID-19 restrictions.
“For more than a year, COVID-19 was the primary cause of respiratory illness in the U.S., but since restrictions were relaxed, it is important for clinicians to consider that other respiratory pathogens may be causing spikes in disease outside of their usual seasonal peaks,” Long said. “The study clearly demonstrates the utility of masks and social distancing and the effect these non-pharmacologic precautions had on suppressing all respiratory viruses, not just COVID-19.” The researchers are now turning their attention to influenza and what to expect next with COVID-19, keeping an eye on whether we’ll see a dual threat of COVID-19 and flu. “It’s too early to say for certain what to expect during the next flu seasons,” Long said.
As Europe experienced its fifth surge in COVID-19 infections in the fall of 2021, Long encouraged the community to get both their COVID-19 and flu vaccines as soon as possible to be prepared because influenza has a history of making healthy people severely ill.
Long’s collaborators in the Center for Molecular and Translational Human Infectious Diseases Research at Houston Methodist Research Institute and the Department of Pathology and Genomic Medicine at Houston Methodist Hospital are Randall J. Olsen, MD, PhD, David W. Bernard, MD, PhD, Paul A. Christensen, MD, Parsa Hodjat, MD, and Sishir Subedi.
To track Houston Methodist’s influenza and other respiratory virus stats, visit http://flu.houstonmethodist.org.
03
Research
Gov. Abbott Visits Houston Methodist
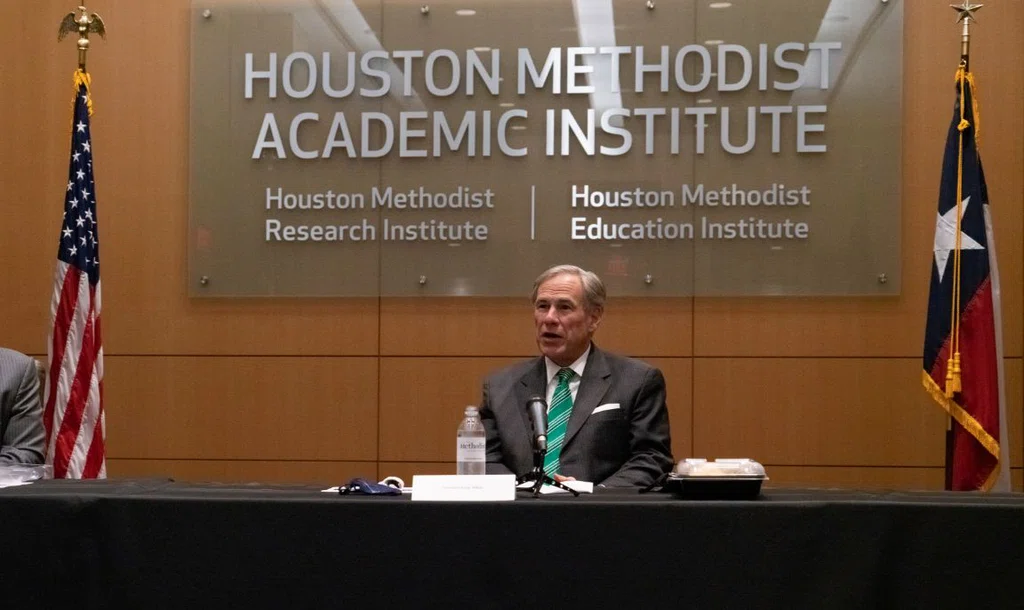
On Tuesday, Jan. 19, 2021, Texas Gov. Greg Abbott visited Houston Methodist, where he hosted a news conference on COVID-19 issues. Abbott shared how impressed he was with Houston Methodist’s efforts. Houston Methodist was chosen for this visit because of its exceptional work throughout the pandemic. Houston Methodist collectively has improved outcomes for COVID-19 patients while reducing hospitalizations overall throughout the course of the pandemic.
In addition to being the first hospital in the country to use convalescent plasma, Houston Methodist also has conducted numerous clinical trials for newly developed treatments, including administering such a high volume of monoclonal antibody treatments that it now orders directly from the distributor. Houston Methodist was chosen as one of the original 28 state hubs to help vaccinate the public.
More from Discovery to Clinic












