President’s Letter
2023 Metrics
Cycle of Translation
Visionary Gifts

Discovery to Clinic

Innovative Education

Translational Luminaries
Introduction
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
Houston Methodist Dr. Mary and Ron Neal Cancer Center
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
COVID-19 Studies
Outcomes Research
Restorative Medicine
Houston Methodist Advances Research into Neural Prosthetics
Noninvasive Spinal Stimulation Works to Restore Movement After Spinal Cord Injury
An Innovative Approach to Treat Even the Most Stubborn-to-Heal Fractures
Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection
Houston Methodist, Rice University, Baylor College of Medicine Design Noninvasive Tech to Help Remove Brain’s Metabolic Waste
Houston Methodist Investigators Nanotechnology Investigators Awarded Prestigious Grants from the Department of Defense
Precision Medicine
Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy
Novel Drug Combination Can Target Triple-Negative Breast Cancer for Treatment
A Houston Methodist and Purdue University Breakthrough May Result in a More Effective Tuberculosis Vaccine
Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease
New Virtual Intensive Care Unit Simultaneously Improves Patient Care and Bed Capacity
result
Introduction
Joint Weill Cornell–Houston Methodist Academic Institute Doctoral Program Welcomes its Inaugural Class
Visionary EnMed Program Soars to New Heights
Neural Control of Organ Degeneration and Regeneration (NeuralCODR) Training Program
Faculty and Research Development
Graduate Medical Education



Science in Service
of
Medicineresult
President's letter
2021 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

From Discovery to Clinic


What is "Discovery to Clinic"?

Restorative Medicine


Houston Methodist Advances Research into Neural Prosthetics

Noninvasive Spinal Stimulation Works to Restore Movement After Spinal Cord Injury

An Innovative Approach to Treat Even the Most Stubborn-to-Heal Fractures

Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection

Houston Methodist, Rice University, Baylor College of Medicine Design Noninvasive Tech to Help Remove Brain’s Metabolic Waste

Houston Methodist Investigators Nanotechnology Investigators Awarded Prestigious Grants from the Department of Defense

Precision Medicine


Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy

New Virtual Intensive Care Unit Simultaneously Improves Patient Care and Bed Capacity

Novel Drug Combination Can Target Triple-Negative Breast Cancer for Treatment

A Houston Methodist and Purdue University Breakthrough May Result in a More Effective Tuberculosis Vaccine

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

Translational Luminaries




Discovery to Clinic

Precision Medicine
Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy
Cancer Cell Type (Seed) and Tumor Microenvironment (Soil) Control Therapeutic Antibody Delivery and Efficacy
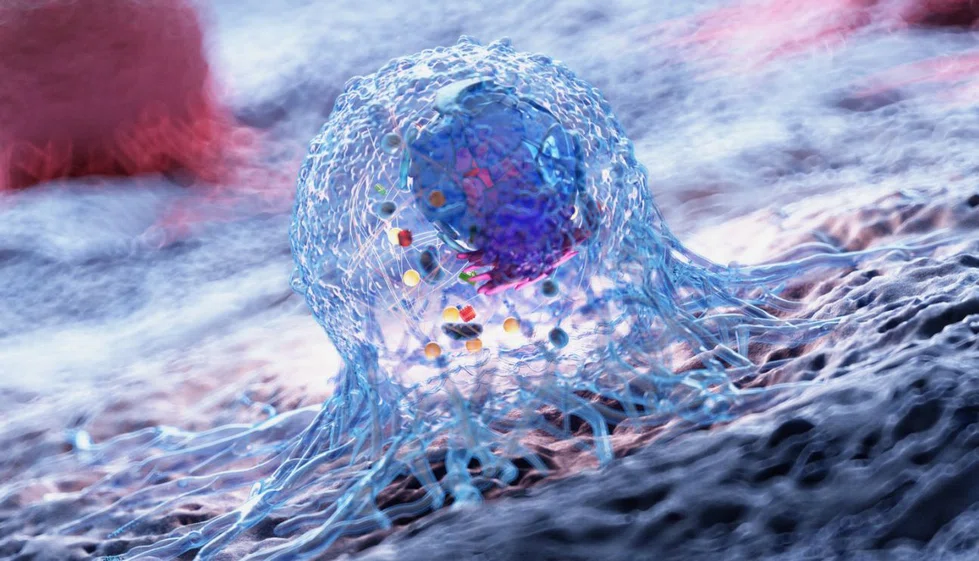
English surgeon Stephen Paget (1855-1926) was the first to propose the “seed and soil” theory of metastasis, which posits that cancer distribution during metastasis is affected by the tumor microenvironment (TME), the organ microenvironment (soil) and the cancer type (seed). Houston Methodist researchers are shining new light on how TME can be used to design personalized therapies and develop novel therapoutics.
There are many variations between cancer cell types (seeds) as well as various theories on how the TME communicates with the metastatic organs (soil). These variations determine where the tumor metastasizes. Most malignant tumors show a preference for metastasizing to a specific organ, although some tumors, such as breast cancer, metastasize to several different organs.
Diversity within the TME influences therapeutic efficacies and the delivery of systemic chemotherapeutics and immunotherapies. For example, drug delivery-based therapeutic resistance comes into play when delivery of chemotherapeutics into cancer cells is below the threshold levels required for biological effect. Another example is the metastasized tumor’s poor response to immune checkpoint inhibitors (ICIs), which are anti-cancer drugs that bind to programmed death-ligand 1 (PD-L1) and are meant to kill the malignant cells in various cancers, including breast cancer. This poor tumor response leads to limitations in chemotherapeutics, particularly breast cancer therapeutics. Although researchers haven’t yet determined precisely why this is the case, it’s been suggested that heterogeneous tumor and microenvironment types play a central role. The correlation between ICI delivery and therapeutic efficacy will be further investigated in future studies.

Kenji Yokoi, MD, PhD
It is critical that researchers better understand the complexity and diversity of the TME to develop novel therapeutics and personalized therapies. To this end, Kenji Yokoi, MD, PhD, associate professor of nanomedicine at Houston Methodist, and his team members established single cell-derived clones from 4T1 murine breast cancer cells and produced orthotopic primary and liver metastasis murine models. Using these models, Yokoi conducted experiments to better understand polyclonal cancer cells and the response of tumors to ICIs.
Notably, in his recent research study published in Pharmaceutics, Yokoi and his research group were the first to suggest a seed and soil-dependent variation in anti-PD-L1 therapeutic delivery and efficacy. Variations were even more pronounced in the liver metastases compared with primary tumors. Interestingly, the clone-dependent variations in PD-L1 expression and anti-PD-L1 IgG delivery were also dependent on tumor location. Using noninvasive fluorescently labeled anti-PD-L1 antibodies, Yokoi demonstrated a high antibody accumulation in tumors with high PD-L1 expression and limited uptake in tumors with low or undetectable PD-L1 levels.


“Phenotypic in vivo therapeutic study and imaging analysis of tumors established from single cell-derived clones growing in different organs may elucidate the specific driving forces in creating a heterogenous response to anti-PD-L1 IgG therapy.”
Kenji Yokoi, MD, PhD
Taken together, Yokoi’s investigations shed more light into understanding the cellular array within the TME and how this diversity affects metastases, which are responsible for most cancer deaths.
More from Discovery to Clinic