Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

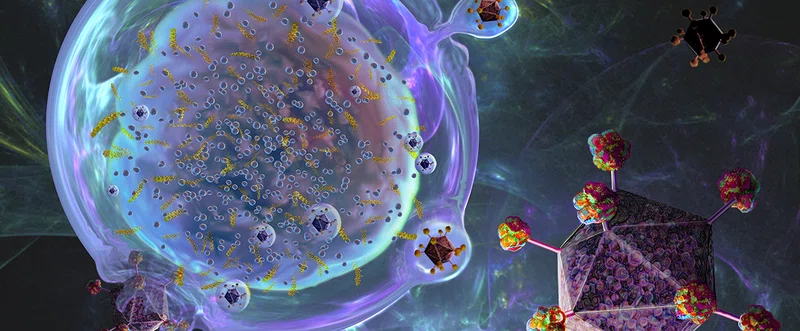
The NanoLymph: Implantable. Adaptable. Anti-cancer




Discovery to Clinic

Precision Medicine

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment
Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment
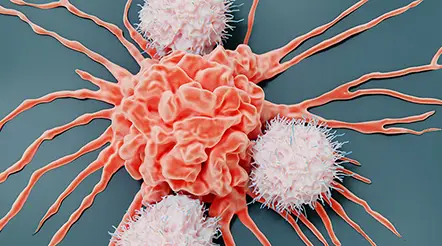
A cancer patient’s T cells, engineered to carry a receptor found on the surface of malignant cells, can aggressively attack tumors — with the potential to revolutionize solid tumor treatment. This technique, referred to as chimeric antigen receptor (CAR) T cell immunotherapy, is useful for various cancers. However, the biggest hurdle is the relapse seen in most patients. A relapse can even be seen in patients with complete remission during early treatment stages. Hence, there is a pressing need to enhance the therapeutic efficacy of CAR-T cells to achieve long-term remissions.
Among other factors, the starting state of T cells determines whether the CAR-T cell immunotherapy will be successful or not. Qing Yi, MD, PhD, the Ralph O’Connor Centennial Chair, Dr. Mary and Ron Neal Cancer Center and Professor of Cancer Biology in Medicine, created interleukin 9 (IL-9) secreting CAR-T cells with a superior anti-tumor potency against CD19-expressing acute lymphoblastic leukemia and GPC3-expressing liver carcinoma.
To unravel the mechanisms behind this, gene set enrichment analysis (GSEA) was performed to evaluate expression levels of genes associated with cell death, cell cycle and proliferation. Results suggested a fivefold higher proliferative capacity and reduced cell death in these T cells compared with T cells grown under different culture conditions (T1 cells).

Our findings highlight a promising clinical potential of human IL-9 secreting T cells for CAR-T cell immunotherapy for human cancers, attributed to their central memory phenotype and that they are less exhausted, hyperproliferative and long-lived in vivo. The unique features of T9 CAR-T cells endow them with greater potential for clinical immunotherapy, which can lead to increased frequency of complete remission, high survival rates, and decreased number of patient relapse after treatment.


Qing Yi, MD, PhD
CAR-T cell immunotherapy hasn’t been terribly successful in solid tumors owing to poor migration and infiltration of CAR-T cells into tumors. In addition to in vitro assays (performed outside a living organism), Yi tested the capacity of human T9 CAR-T cells to repress solid tumor growth in murine tumor models. Tumor-bearing mice treated with T9 CAR-T cells showed greater T9 CAR-T cell infiltration into tumor sites, greater survival, and reduced tumor growth compared with T1 CAR-T treated mice. Thus, T9 CAR-T cells show considerable therapeutic efficacy and potential for solid human tumors.
According to Yi, “Our findings highlight a promising clinical potential of human IL-9 secreting T cells for CAR-T cell immunotherapy for human cancers that are attributed to their central memory phenotype and are less exhausted, hyperproliferative and long-lived in vivo. The unique features of T9 CAR-T cells endow them with greater potential for clinical immunotherapy, which can lead to increased frequency of complete remission, high survival rates, and decreased number of patient relapse after treatment.”
Treatment outcomes in solid and liquid tumor patients can be significantly enhanced by harnessing the hyperproliferative capacity and robust antitumor potency of human T9 CAR-T cells. Engineering T cells with a CAR is justifiable and human T9 CAR-T cell therapy is likely to lead to better long-term remission among cancer patients.