Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


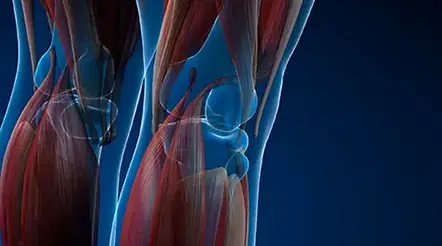
Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer





Discovery to Clinic

Restorative Medicine
Novel Vascular Engineering Platforms are a Boon for Bioengineering
Novel Vascular Engineering Platforms are a Boon for Bioengineering

As of December 2022, more than 104,000 people in the U.S. are waiting for a life-saving organ transplant. Every nine minutes, another person is added to the transplant waiting list, and 17 people die each day waiting for a transplant. The dearth of donated organs has inspired scientists to investigate the application of bioengineering principles to generate human organs in the lab.
Bioengineered organs could potentially not only replace donor organs but also provide an unlimited supply. In addition, there would be no immune suppression required, improving success rates of transplant surgeries. The field of bioengineered organs has been advancing at a steady pace, but Houston Methodist’s Joan Nichols, PhD, the Dr. and Mrs. Alan L. Kaplan Centennial Professor in Cellular Therapeutics and Organ Bioengineering in the Department of Surgery and Professor of Immunology in Surgery, and her team have made a breakthrough in organ engineering that brings clinical translation one step closer to reality and can be easily adapted to many other applications.

Joan Nichols, PhD
Bioengineering of a whole organ requires a scaffold upon which the cells can grow, develop and function. In a complex organism, this role is filled by the extracellular matrix. For bioengineering, a biological scaffold is generated by decellularization of naturally occurring human or animal tissues and organs. Removing the cells removes the allogeneic and xenogeneic cellular antigens, thus eliminating the immune response that would lead to organ rejection.
In 2018, Nichols’ team published a paper in Science Translational Medicine revealing their success with a bioengineered lung that was transplanted in a clinically relevant preclinical model. And while their model functioned to produce systemic vascular circulation, it was not suitable for development of functional pulmonary circulation with bioengineered pulmonary artery and vein. Nichols attributed the lack of vascular tissue development to limited dispersal of the growth factor needed for vascular tissue development — vascular endothelial growth factor (VEGF) — and other additives in the whole organ scaffold, combined with the inability of the system to retain the growth factor delivery suspension within the scaffold framework. VEGF is critical in vascular development and has been shown to support development of vascular tissue in bioengineering, but it needs to attach to the scaffold and remain in place to do the job.
Generating vascular tissue with microvasculature networks capable of perfusion at physiological pressures without leaking is perhaps the most common challenge in organ and tissue bioengineering. The biomimetic vascular models available have been unable to model vascular cell responses and lacked the appropriate vascular culture platforms focused on three-dimensional whole vessel or whole lung vascular bioengineering. While microfluidic-supported platforms are the standard for investigating endothelial cell culture methods and vascular tissue responses, they are unable to accommodate evaluation of whole vessel or whole organ culture.
So, Nichols’ group did what they do best and developed what they needed to advance their work: novel in vitro biomimetic vascular models with appropriate culture- or microfluidic-supported vascular platforms to assess vascular cell responses to growth factors and factor delivery vehicles. These platforms include flattened pieces of vascular scaffold with standard plate culture; microfluidic system-supported whole-vessel scaffolds and whole acellular lung scaffolds. The whole vessel and whole lung platforms are microfluidic-supported culture chambers that mimic native tissue function to allow medium exchange and provide nutrient and oxygen circulation and waste removal from the culture micro-environment.
The Nichols' lab team (left to right): Lissenya Argueta, PhD, Postdoctoral Research Fellow, Joan Nichols, PhD, Director, Center for Tissue Engineering, Sasha Azar, PhD, Assistant Professor and Jean Niles, Research Associate III.
In the study published last summer in Nanomedicine: Nanotechnology, Biology and Medicine, Nichols’ team used these platforms to investigate delivery of VEGF via microparticle (MP) or hydrogel vehicles to the scaffolds and the effects of VEGF on vascular cell attachment and subsequent tissue formation in in vitro bioreactor culture. Their results are exciting for several reasons.
In vivo imaging of their system shows that VEGF-MP size and shape allowed retention in the mesh-like collagen/elastin network comprising the acellular whole-lung scaffold but did not impede MP dispersal through its vascular tree. Importantly, they detected no evidence of VEGF-MPs or degraded VEGF-MPs outside of the vascular scaffold, and particles were distributed throughout whole left lung scaffolds including in the small capillary regions. Ten days post culture, VEGF could be detected in degrading VEGF-MPs. The effects of VEGF on the scaffolds: endothelial cell attachment and microvascular and vascular tissue formation, were found only in the MP-targeted vascular regions. In addition, they found that a 50/50 mixture of 30 and 60 nm pore-sized silicon wafer MPs was superior to the hydrogel for delivering VEGF. While hydrogels are thermosensitive and cannot provide slow, controlled release of growth factors, MPs with the appropriate pore size provide temporospatial release of factors to facilitate both protein loading and load release. Furthermore, they demonstrated that MPs could fit into even the smallest vascular regions and in whole organ scaffolds. These results show that MPs are more effective than hydrogel at delivering bioactive factors in acellular whole lung scaffolds to facilitate vascular tissue bioengineering.
The success of silicon MPs for factor delivery is especially exciting for the future of vascular and organ bioengineering because standardization of pharma-grade MPs can be achieved by leveraging well-characterized large-scale manufacturing techniques borrowed from the semiconductor industry. These techniques have the scalability to support research and development studies, clinical trials and, ultimately, clinical commercial use.
Their results also demonstrate that the newly developed platforms provide the modeling capabilities researchers in this field need to keep advancing their work. These platforms not only signal important advancement for whole organ and vascular bioengineering; they can also be adapted for use in other studies. Additionally, they allow assessment of growth factors (alone or in combination) and delivery systems that can be easily modified to evaluate therapeutics for clinical vascular graft production, vascular regeneration, vascular health and more.
Currently, Nichols and her team are working on using these platforms to model select agent and SARS-CoV-2 infections and test candidate countermeasures.
More from Discovery to Clinic