Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer




Discovery to Clinic

Clinical Research

Houston Methodist Conducts First-Ever Study into a Challenging Situation
Houston Methodist Conducts First-Ever Study Into a Challenging Situation
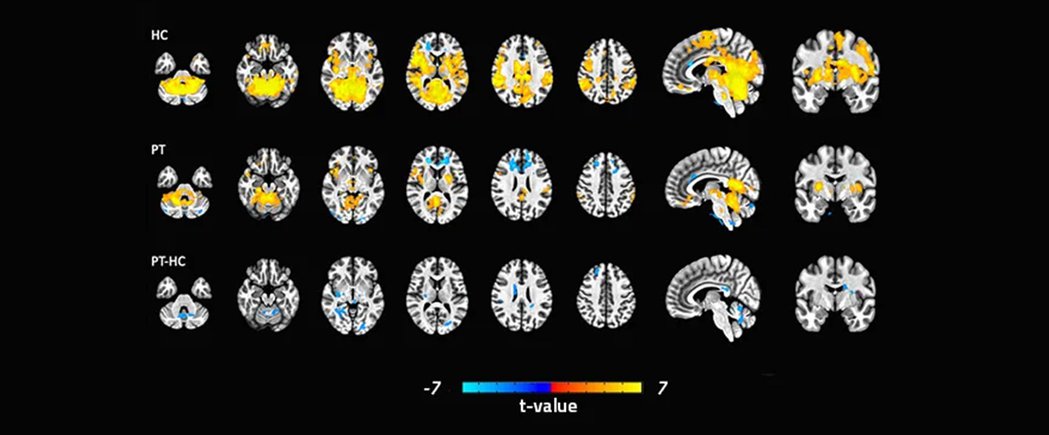
Functional defecatory disorder (FDD) is a challenging condition for patients and clinicians alike, but a new study that shows differences in related activation patterns of patients' brains may help streamline diagnosis and treatment, offering faster relief.
Characterized by a frequent and powerful urge to evacuate one's bowels and an inability to effectively do so, FDD primarily affects women and can lead to chronic constipation, pain, disruption to daily life and even hospitalization.
The study, published in Neurogastroenterology & Motility, is the first of its kind to investigate the central control mechanism of defecation in humans using concurrent functional MRI recording and rectal manometry.
"Until now, research on functional defecatory disorder has concentrated almost exclusively on colorectal anatomy and peripheral mechanisms," said Eamonn Quigley, MD, Director of the Underwood Center for Digestive Disorders and co-author of the study.

Eamonn Quigley, MD
"Likewise, clinicians and patients can spend months seeking and ruling out physical causes, using expensive and sometimes invasive tests. This study offers compelling evidence that we should be focusing on the brain-gut connection and brain-directed therapies for the highest chance of success.
“There were differences in key regions of the brain that have to do with executive-cognitive function, coordination and emotion, which suggests some lack of communication and/or coordination between the brain and the pelvic floor and sphincter muscles. But it doesn't necessarily explain how or why this occurs. Are these individuals receiving the wrong signals from down below or are they sending the wrong signals down below, or does it go both ways? Is it caused by psychological stress or is the person's functional defecatory disorder causing them psychological stress?" asked Quigley.
To investigate the brain-gut connection, researchers recruited 15 healthy female control subjects and 18 women with FDD to undergo a balloon expulsion test and functional MRI at the same time. The goal: identify the specific regions of the brain involved in defecation and determine if activity in these regions is different in FDD. Such activity was measured by blood-oxygen-level-dependent (BOLD) signals.
Simulated defecation was associated with activation of regions of primary and supplementary motor and somatosensory cortices, homeostatic afferent (thalamus, mid-cingulate cortex and insula) and emotional arousal networks (hippocampus and prefrontal cortex), occipital and cerebellum along with deactivation of right anterior cingulate cortex (ACC) in controls.
Study participants with FDD had fewer brain regions engaged during defecation and significantly decreased BOLD signals in areas related to executive-cognitive function (insula, parietal and prefrontal cortices). They showed higher activation in the right ACC than healthy study participants. Otherwise, brain activation patterns were similar when tightening the anal sphincter.
Although further research is needed to explore these questions, the study's important insight, according to Quigley, is that the brain plays a critical role in medicating this process. This provides further validation for the role of brain-directed therapies like biofeedback as the mainstay of treatment for FDD.
"Achieving an effective bowel movement is more complicated than most people realize," Quigley said. "It requires the subtle coordination of a variety of muscles, the nerves that supply those muscles, the brain and the signals the brain is sending to either contract or relax."
Biofeedback is a form of physical therapy that uses neuromuscular conditioning techniques to coach patients on the dynamics of defecation. Studies have shown it is effective in up to 80% of patients with FDD.
"I hope physicians will review our study and feel empowered to recommend biofeedback right out of the gate, rather than feeling the need to go down all the other potential avenues first," Quigley said. "Retraining the mind and body takes time, but it offers real relief for a condition that significantly impacts quality of life."