Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

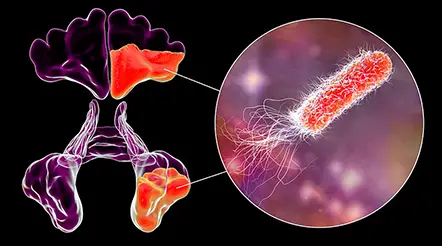
COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer





Discovery to Clinic
Clinical Research

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?
Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?
Nhat-Tu Le, PhD, Associate Professor of Cardiovascular Sciences, suggests a novel approach for future therapies for both cancer and cardiovascular diseases (CVDs) by pinpointing senescence-associated secretory phenotype (SASP) as a key modulator of both.
The link between cellular aging and disease development is a key point of convergence where Houston Methodist researchers are developing an intervention that can slow or perhaps even reverse the progression of both cancer and cardiovascular disease. While research in the fields of CVD and cancer have made considerable advancements in prevention, screening, and treatment, these diseases continue to be the leading causes of death across the world. Researchers at Houston Methodist have made a surprising discovery leading to the development of technology with the ability to rejuvenate human cells.
Nhat-Tu Le, PhD
Risk factors common to both diseases include smoking, obesity, older age, diabetes, gender, family history, hypertension, sedentary lifestyle, unhealthy diets and the gut microbiome. This extensive list of shared risk factors suggests a commonality in how these two diseases manifest in the human body. CVD and cancer can coexist in the same individual. Patients with CVD are at an elevated risk of developing cancer, and conversely, those with cancer (particularly lung, breast and colon cancer) are at a higher risk of developing CVD.
Research on cancer and CVD development has demonstrated senescence — the process of biological aging — to be a common link in the connection between these two disease progressions. Senescence (derived from the Latin word “senex” meaning “old”) was originally discovered serendipitously by Leonard Hayflick in 1961.
Albeit in a state of cell cycle arrest, senescent cells can remain metabolically active and secrete cytokines, chemokines, growth factors and reactive oxygen species (ROS). This SASP is induced by myriad stressors, including cancer treatments, pro-inflammatory cytokines and ROS. Although the precise role of senescence in the intersection of CVD and cancer development is unclear, SASP is hypothesized to be involved.
In a review study published in Frontiers in Cardiovascular Medicine in 2021, Le detailed how SASP instigates CVD and the molecular mechanisms by which SASP is implicated in tumorigenesis. The functional role of senescence in cancer is controversial. SASP can be induced in both normal and cancer cells by stress, oncogenes or therapy. Interestingly, chemotherapy-induced senescence can condition senescent cancer cells to acquire senescence-associated stemness, which causes them to escape cell cycle arrest, become proliferative and promote both CVD and cancer. On the other hand, several murine model and human specimen studies have demonstrated that senescent cardiovascular cells accumulate at the site of CVD and promote atherosclerosis, heart failure, arterial stiffness and hypertension.
A key observation noted by Le is that SASP can lead to CVD as well as cancer. Conversely, both cancer and CVD provide feedback loops to activate SASP.
Understanding the regulation of SASP is the key to understand not only the interconnections between cancer and CVD but also age-related diseases such as diabetes mellitus, Alzheimer’s disease, cataract and chronic obstructive pulmonary disease.
Nhat-Tu Le, PhD
In a review study published in Frontiers in Cardiovascular Medicine in 2021, Le detailed how SASP instigates CVD and the molecular mechanisms by which SASP is implicated in tumorigenesis. The functional role of senescence in cancer is controversial. SASP can be induced in both normal and cancer cells by stress, oncogenes or therapy. Interestingly, chemotherapy-induced senescence can condition senescent cancer cells to acquire senescence-associated stemness, which causes them to escape cell cycle arrest, become proliferative and promote both CVD and cancer. On the other hand, several murine model and human specimen studies have demonstrated that senescent cardiovascular cells accumulate at the site of CVD and promote atherosclerosis, heart failure, arterial stiffness and hypertension.
A key observation noted by Le is that SASP can lead to CVD as well as cancer. Conversely, both cancer and CVD provide feedback loops to activate SASP.
“Understanding the regulation of SASP is the key to understand not only the interconnections between cancer and CVD but also age-related diseases such as diabetes mellitus, Alzheimer’s disease, cataract and chronic obstructive pulmonary disease,” said Le.
Cancer treatments improve patient survival. However, the side effects can decrease patients’ quality of life. In many cases, the cancer cells become resistant to therapies and evolve to become even more aggressive, which defeats the purpose of the therapy. One interesting case in point is the strategy used in therapy-induced senescence whereby the therapy triggers cellular senescence to impede the growth of cancer cells. Surprisingly, therapy-induced senescence can induce SASP, which can lead to more potent cancer growth. Strategies focusing on modulating SASP appear to hold greater promise in the future for advances in the treatment of both CVD and cancer.