Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

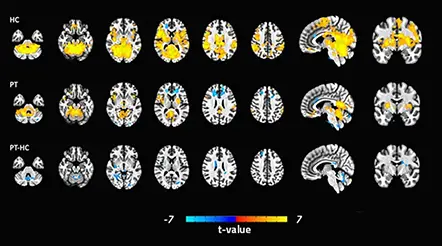
COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer





Discovery to Clinic
Clinical Research

Improving Treatment Options for Patients with Severe Retinal Vascular Disease
Improving Treatment Options for Patients with Severe Retinal Vascular Disease
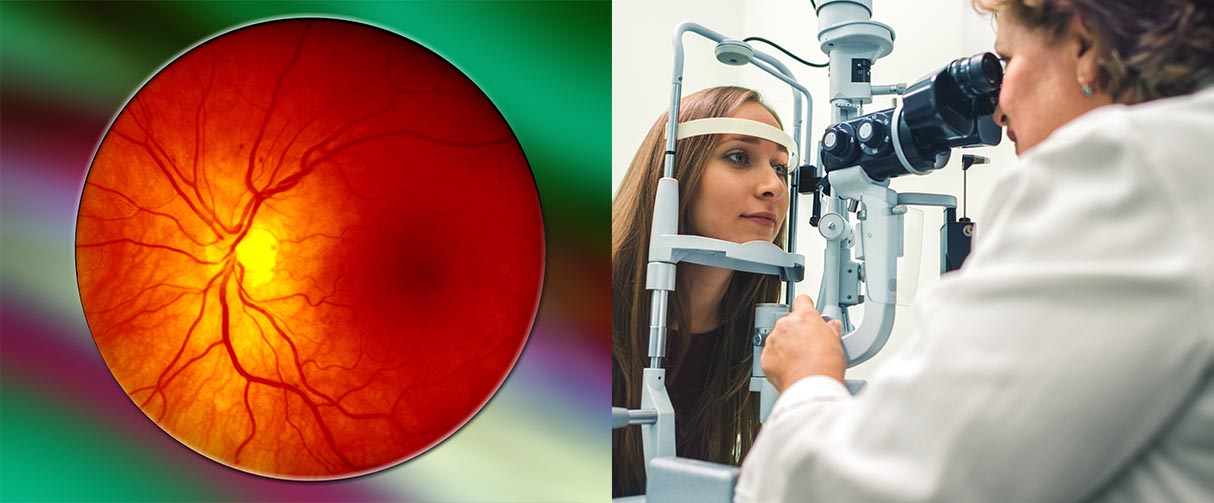
A new drug, faricimab, recently received FDA approval for the treatment of diabetic macular edema and neovascular age-related macular degeneration following the publication of primary results in four major phase 3 clinical trials, as reported in The Lancet.
The researchers demonstrated that faricimab met noninferiority endpoints over a current drug, aflibercept, while demonstrating robust vision gains, anatomical improvements and potentially longer intervals between dosing.

Charles Wykoff, MD, PhD
“It’s quite unusual to obtain simultaneous FDA approval for two common diseases, and I think it speaks to how well suited this particular drug is for the job of treating exudative retinal diseases,” said Charles Wykoff, MD, PhD, a Houston Methodist ophthalmologist and the principal investigator of the two nearly identical diabetic macular edema trials, YOSEMITE and RHINE.
Diabetic macular edema and neovascular age-related macular degeneration are the leading causes of irreversible blindness in the U.S., with 4 million adults actively affected and 10 million more at risk of severe retinal vascular disease. Both diseases are characterized by abnormal blood vessels that leak in the retina, causing a buildup of fluids and consequently a progressive loss of vision.
The most common treatment to arrest blood seepage is antivascular endothelial growth factor A (anti-VEGF-A) medications that are delivered into the eye by intravitreal injection. These drugs have been a remarkable breakthrough, said Wykoff, changing the epidemiology of blindness and the prognosis of patients with diabetic macular edema and neovascular age-related macular degeneration.
Despite the effectiveness of anti-VEGF-A medications, certain drawbacks made treatment adherence and widespread adoption a significant challenge.
“Patients require an injection typically every four to 12 weeks, often indefinitely,” said Wykoff. “That is a substantial burden for patients, caregivers and eye care providers alike and a limitation of current therapeutics that has prevented us from fully realizing the potential of these drugs in the real world. Many of these patients face significant comorbidities and mobility issues related to advanced age or conditions associated with diabetes.”
Unlike anti-VEGF-A medications that target a single biochemical signaling pathway, faricimab, an angiopoietin-2 and VEGF-A bispecific antibody, blocks two key signaling pathways that are implicated in the pathogenesis of diabetic macular edema and neovascular age-related macular degeneration. In particular, by inhibiting angiopoietin-2, native angiopoietin-1 can bind to the endothelial receptor tyrosine kinase transmembrane receptor Tie2, leading to increased intracellular signaling that improves vascular leakage and drives stabilization of the blood-retinal barrier, reductions in inflammation and improved cell survival.
In preclinical studies and three phase 2 clinical trials concluded in 2019, the dual pathway inhibition demonstrated the potential for increased vascular stability and greater reductions in vascular leakage, neovascularization and inflammation over VEGF-A inhibition alone.

It’s quite unusual to obtain simultaneous FDA approval for two common diseases, and I think it speaks to how well suited this particular drug is for the job of treating exudative retinal diseases.
Charles Wykoff, MD, PhD
“We wanted to test the durability of this novel drug using methods common in clinical practice, where you treat consistently until you achieve optimal outcomes, then titrate the frequency to meet individual patient needs,” explained Wykoff.
The diabetic macular edema trials were the first to incorporate a flexible, individualized treatment interval-approach in a double-masked manner. Nearly 1,900 patients across 353 sites worldwide were randomly assigned to receive either (a) faricimab every eight weeks, (b) aflibercept (a VEGF-A antagonist) every eight weeks, or (c) faricimab per personalized treatment intervals.
By the end of the one-year study period, more than 50% of patients in the personalized treatment interval groups could go up to 16 weeks between treatments without losing vision gains, and 70% could go up to 12 weeks or longer.
Faricimab, the researchers found, produced a more sustained effect than anti-VEGF-A monotherapies, like aflibercept, with faricimab demonstrating efficacy at up to 16-week intervals. In the future, additional studies are planned to examine the potential to extend treatment intervals even further in some patients.
In parallel, neovascular age-related macular degeneration phase 3 clinical trials, TENAYA and LUCERNE, led by Jeffrey Heier from Ophthalmic Consultants of Boston, 80% of patients receiving faricimab maintained their best-corrected visual acuity at 12-week or longer intervals, with 45% maintaining it at 16-week intervals.
In January, Vabysmo (faricimab-svoa) became the only injectable eye medicine approved simultaneously in the U.S. for diabetic macular edema and neovascular age-related macular degeneration, with flexible dosing regimens based on patient need. Vabysmo is manufactured by Genentech, a subsidiary of F. Hoffmann-La Roche, who provided funding for the studies.
More from Discovery to Clinic

A New FDA-Approved Treatment for Sufferers of Chronic Constipation
A capsule designed to vibrate in the GI tract to stimulate the bowels accelerates movement in the field of chronic constipation.