Introduction
Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist
Houston Methodist Dr. Mary and Ron Neal Cancer Center
The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative
Houston Methodist Cockrell Center for Advanced Therapeutics
Paula and Joseph C. “Rusty” Walter III
Translational Research Initiative
Jerold B. Katz Academy of Translational Research
Infectious Diseases Research Fund
George and Angelina Kostas Research Center for Cardiovascular Medicine
New Endowed Chairs Positions
EnMed
Center for Bioenergetics
result
Clinical Research
Outcomes, Quality and Healthcare Performances
Restorative Medicine
Precision Medicine
Science in Service
of
Medicineresult
President's letter
2022 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer





Discovery to Clinic
Precision Medicine

COVID-19 Infection in Crucial Brain Regions May Lead to Accelerated Brain Aging
COVID-19 Infection in Crucial Brain Regions May Lead to Accelerated Brain Aging

Since SARS-CoV-2 infection was first detected in humans in December 2019, the disease, through the virus’ many variants, continues to pose a serious threat to global health. While the respiratory symptoms are more well known, COVID-19’s deleterious effects on other organs in the human body are being actively investigated.
In a new Ageing Research Reviews article, Houston Methodist researchers have consolidated the emerging insights and evidence that suggest COVID-19 infections may have both short- and long-term neurological effects. Major findings include that COVID-19 infections may predispose individuals to develop irreversible neurological conditions, may increase the likelihood of strokes, and may increase the chance of developing persistent brain lesions that can lead to brain bleeding.

Muralidhar Hegde, PhD
“Microhemorrhages caused by SARS-CoV-2 infections in crucial brain regions can speed up brain aging in COVID-19 survivors and can also lead to complex and irreversible neurodegenerative conditions that can severely impact cognitive and motor functions,” said corresponding author Muralidhar Hegde, PhD, the Everett E. and Randee K. Bernal Centennial Endowed Director of DNA Repair and Professor of Neurosurgery with the Center for Neuroregeneration at Houston Methodist.
Still a major burden on our daily lives, a great deal of research has shown that the impacts of the disease go far beyond the actual time of infection. Since the onset of the pandemic, COVID-19 has surpassed a death toll of more than 5.49 million worldwide and over 307 million confirmed positive cases, with the U.S. accounting for almost 90 million of those cases, according to the Our World in Data website.
COVID-19 has numerous impacts on the central nervous system. For instance, 20% to 30% of COVID-19 patients report a lingering psychological condition known as “brain fog” where individuals suffer from symptoms such as memory loss, difficulty in concentrating, forgetting daily activities, difficulty in selecting the right words, taking longer than usual to complete a regular task, disoriented thought processes and emotional numbness.
The coronavirus infection can cause long-term and irreversible damage to the brain, particularly in the elderly and other vulnerable populations. Several brain imaging studies on COVID-19 victims and survivors have confirmed the formation of microbleed lesions in deeper brain regions involved in cognition and memory. In this review, researchers have critically evaluated the possible chronic neuropathological outcomes in aging and comorbid populations if timely therapeutic intervention is not implemented.
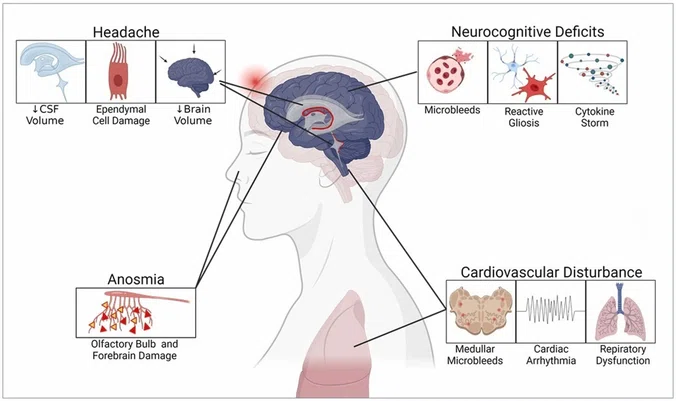
Cerebral microbleeds are emerging neuropathological signatures frequently identified in individuals suffering from depressive syndromes, chronic stress, type 2 diabetes, and other age-associated comorbidities. Based on their earlier findings, the Houston Methodist investigators discussed how COVID-19-induced microhemorrhagic lesions may exacerbate DNA damage in affected brain cells, resulting in neuronal senescence and activation of cell death mechanisms that ultimately impact brain microstructure-vasculature. These pathological phenomena resemble the hallmarks of neurodegenerative diseases such as Alzheimer’s and Parkinson’s and are likely to aggravate advanced-stage dementia as well as cognitive and motor deficits.
“Importantly, individuals over the age of 60 with preexisting neuropathological conditions might be at the highest risk of developing chronic neurodegeneration,” said Joy Mitra, PhD, an instructor with the Center for Neuroregeneration and lead author of the study.
More severe long-term effects following COVID-19 infection include predispositions for Alzheimer’s, Parkinson’s and related neurodegenerative diseases as well as cardiovascular disorders due to internal bleeding and blood clotting-induced lesions in the part of the brain that regulates our respiratory system. Additionally, cellular aging is thought to be accelerated in COVID-19 patients. A plethora of cellular stresses inhibit the virus-infected cells from undergoing their normal biological functions and let them enter into “hibernation mode” or even die completely.
The study also suggests various strategies to improve some of these long-term neuropsychiatric and neurodegenerative outcomes as well as outlines the importance of the therapeutic regimen targeting hemorrhage-induced neurotoxicity in combination with various FDA-approved drugs that may prove successful to fight against COVID-19.
However, given the ever-evolving nature of this field, associations like the ones described in this review show the fight against COVID-19 is far from over, noted the investigators, and reinforce the message that getting vaccinated and maintaining proper hygiene are key in trying to prevent such long-term and detrimental consequences.