Share this story




President’s letter
2022 Metrics
Cycle of Translation
Visionary Gifts

Discovery to Clinic

Innovative Education

Translational Luminaries
COVID-19 Studies
Outcomes Research
Restorative Medicine
Houston Methodist and Rice University Launch Center for Translational Neural Prosthetics and Interfaces
Non-invasive Spinal Stimulation Enables Paralyzed People to Stand Unassisted
Dissolvable Implants Enhance the Body’s Ability to Heal Broken Bones
Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection
Revolutionizing the Future of Complex Valve Disease Management
Precision Medicine
CPRIT Funding to Drive New Discoveries in Cancer Therapeutics
Siemens Healthineers and Houston Methodist Imaging Innovation Hub Empowers Researchers to Push the Boundaries
Novel Monoclonal Antibody Treatment Halts Tumor Growth in Deadly Ovarian and Pancreatic Cancers
Houston Methodist Institute for Technology, Innovation & Education (MITIESM)
Can Devices Provide A New Treatment Option for Glioblastoma?
Houston Methodist Hospital’s new Paula and Joseph C. “Rusty” Walter III Tower offers the Most advanced treatments and innovations available
Neuroimaging Offers New Insights into Neurodegeneration
result



Science in Service
of
Medicineresult
President's letter
2020 Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

The Ann Kimball and John W. Johnson Center for Cellular Therapeutics

The Fondren Food & Health Alliance and The Fondren Inflammation Center

Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

From Discovery to Clinic


Introduction

Restorative Medicine


Houston Methodist and Rice University Launch Center for Translational Neural Prosthetics and Interfaces

Non-invasive Spinal Stimulation Enables Paralyzed People to Stand Unassisted

Dissolvable Implants Enhance the Body’s Ability to Heal Broken Bones

Cell Encapsulation May Hold the Key to Preventing Cell Transplant Rejection

Revolutionizing the Future of Complex Valve Disease Management

Precision Medicine


CPRIT Funding to Drive New Discoveries in Cancer Therapeutics



An Innovative New Tool to Enable Drug Discovery and Personalized Medicine


Devising a Novel Combination Treatment for Aggressive Double-hit Lymphoma

Expanding the RNAcore to Encompass the Entire Cycle of a Cure

Siemens Healthineers and Houston Methodist Imaging Innovation Hub Empowers Researchers to Push the Boundaries

Novel Monoclonal Antibody Treatment Halts Tumor Growth in Deadly Ovarian and Pancreatic Cancers

Houston Methodist Institute for Technology, Innovation & Education (MITIESM)


Surgical Technology Developed in MITIE Gains FDA Approval


Pushing the Frontier of the Robotics Revolution

Can Devices Provide A New Treatment Option for Glioblastoma?

Houston Methodist Hospital’s new Paula and Joseph C. “Rusty” Walter III Tower offers the Most advanced treatments and innovations available

Neuroimaging Offers New Insights into Neurodegeneration

Translational Luminaries



Discovery to Clinic

Precision Medicine

Novel Monoclinal Antibody Treatment Halts Tumor Growth in Deadly Ovarian and Pancreatic Cancers
Novel Monoclinal Antibody Treatment
Halts Tumor Growth in Deadly Ovarian and Pancreatic Cancers



A research collaboration between Houston Methodist and The University of Texas MD Anderson Cancer Center has identified a promising new antibody therapy for late-stage ovarian and pancreatic cancers. Termed “silent killers,” these cancers often go undetected until they are too late to treat.
For any tumor, its surrounding environment plays a crucial role in promoting growth and progression. Tumor microenvironment is composed of different types of cells and proteins, each of which influences cancer cell growth, migration and differentiation.
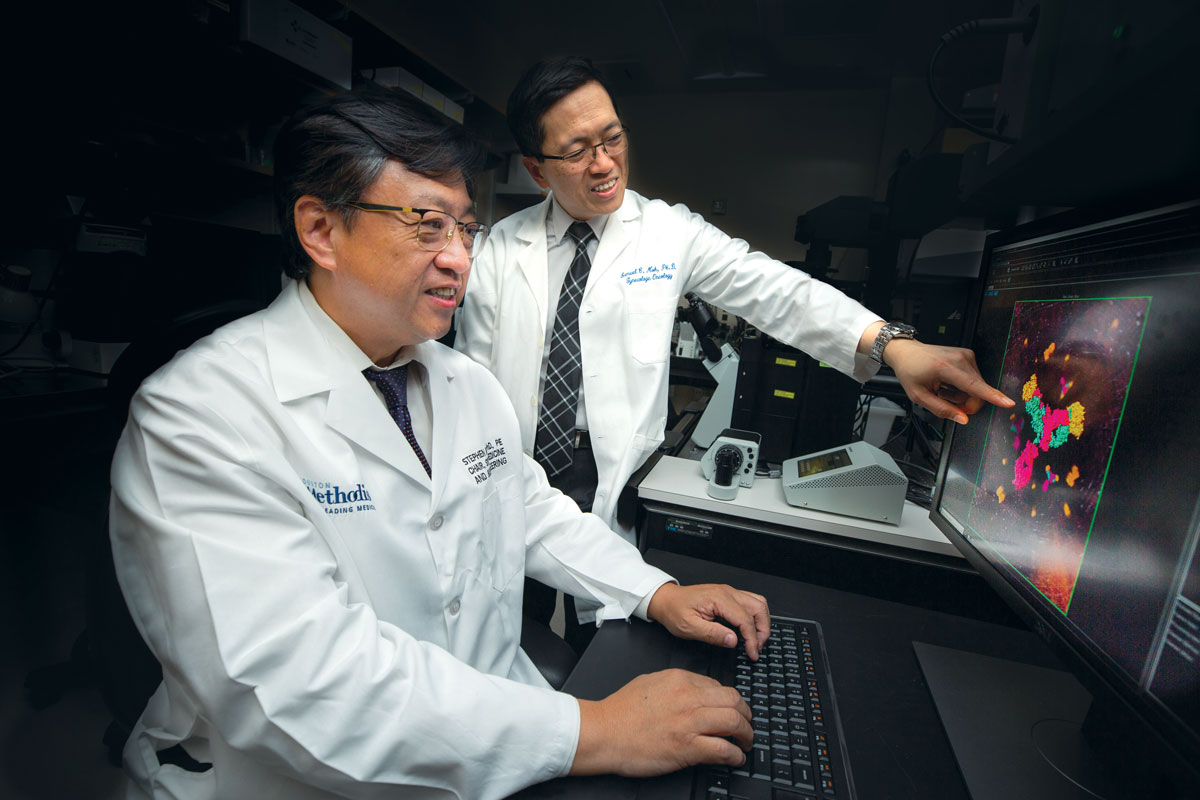
Stephen Wong, PhD, from Houston Methodist Cancer Center, and Samuel Mok, PhD, from The University of Texas MD Anderson Cancer Center, are collaborating to create an antibody as a new type of immunotherapy.
A group of researchers led by Stephen Wong, PhD, from Houston Methodist Cancer Center and Samuel Mok, PhD, from The University of Texas MD Anderson Cancer Center, identified a protein called MFAP5 which was elevated in the tumor microenvironment of both ovarian and pancreatic
cancers. They also showed that MFAP5 plays a crucial role in promoting metastasis of these cancers, stimulating blood vessel formation within the tumor and enhancing cancer cells’ resistance to chemotherapy drugs. This made MFAP5 a promising therapeutic target for treating ovarian and pancreatic cancers.
To test if blocking MFAP5 produced a desirable anticancer effect, Wong and colleagues devised a new monoclonal antibody 130A that successfully blocked MFAP5 in preclinical models of ovarian and pancreatic cancer. Developed and patented by Wong and Mok, the antibody prevented the
formation of new blood vessels within the tumor, thereby cutting off the support needed for tumor growth and proliferation. It also enhanced the bioavailability and effectiveness of other chemotherapy drugs and inhibited tumor growth as well as progression. Most importantly, treatment with the MFAP5-targeting antibody curbed tumor progression without producing noticeable toxic effects. Co-corresponding authors Wong and Mok published their findings in the journal Clinical Cancer Research.
Pinch to zoom image


Wong and Mok created the antibody to block the action of the MFAP5 protein, secreted by the cells that surround and support ovarian and pancreatic tumor cells.
“The lack of side effects can be attributed to the fact that MFAP5 is expressed at very low levels in normal cells compared to cells in the tumor microenvironment, which makes this therapy highly targeted,” said Wong.
After demonstrating the efficacy of their monoclonal antibody in preclinical models, the team’s next step will be to design an anti-MFAP5 antibody that can be used in human studies. According to Wong, this work requires the seamless convergence of expertise across varied disciplines such as biological science, computational science and engineering, making this a truly multidisciplinary effort.

“Finding an effective targeted treatment for two of the most lethal cancers is like the holy grail of cancer research. This translational discovery has raised the prospect of developing a treatment for late-stage ovarian and pancreatic cancers.”
Stephen T.C. Wong, PhD
John S. Dunn, Sr. Presidential Distinguished Chair in Biomedical Engineering Professor of Computer Science and Bioengineering in Oncology Cancer Center
Houston Methodist
More from Discovery to Clinic