Science in Service
of
Medicineresult
President & CEO Letter
2025 Annual Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer

Science in Service
of
Medicine
From the President
2025 Annual Metrics
Cycle of Translation
result
Transplant Battlegrounds

Every transplant is a unique, lifesaving event that can powerfully affect organ recipients, donors and their families. The J.C. Walter Jr. Transplant Center program continues to make indelible impact on the lives of countless patients and families. In 2024, the Center completed 738 transplants across four organs—60 hearts, 90 Lungs, 293 livers, 287 kidneys—and generated 134 living donor transplants and implanted 35 LVADs, bringing the total to 773 end-organ interventions and 134 living donor procedures.
01
Troublesome T Cells
Every day, 17 people die waiting for organ transplants, but getting a new organ doesn’t guarantee survival. Despite immunosuppressive medications, rejection of transplanted organs happens in up to 50% of patients.


50%
Houston Methodist researchers, led by Wenhao Chen, PhD, Associate Professor of Transplant Immunology in Surgery, are advancing the field with the identification of a troublesome subset of CD4+ T cells that may be a more effective therapeutic target for preventing transplant rejection in patients.

Wenhao Chen, PhD
Transplanted tissues and organs are recognized as "foreign" by our immune systems, thereby triggering an immune response that leads to the physiological rejection of the tissue. To prevent this, physicians must modulate immunity for the foreign object to be tolerated, and adjust immune responses. While the molecular pathways leading to T cell activation have been extensively studied, the mechanisms that modulate subsequent CD4+ T cell effector programs resulting in transplant rejection are not fully understood.
To gain deeper insight into the role of CD4+ T cells in transplant rejection, Chen’s study utilized single-cell RNA sequencing to analyze the CD4+ T cell response in transplantation scenarios. The results, published in Nature Immunology, indicate the presence of stemlike CD4+ T cells in transplant recipients, as well as the stem-like program directing the CD4+ T cell response in models of transplantation.
More specifically, they found stem-like CD4+ T cells which recognize transplant antigens that can differentiate into effector cells that attack transplanted organs. However, the effector cells lose their ability to proliferate and fail to reject allografts upon adoptive transfer into new recipients.
These results provide robust evidence for a stem-like program that controls the self-renewal and effector differentiation abilities of CD4+ TEP cells. Because the stem-like CD4+ T cells continually replenish the effector cell pool, they may be the more effective therapeutic target for preventing transplant rejection and in other T cell-related immunotherapies
“The identification of these stem-like CD4+ T cells as a key driver of transplant rejection opens a promising new frontier in clinical transplant care. By targeting these cells specifically, we could enhance our ability to prevent rejection, improve long-term outcomes, and ultimately offer patients a better chance at a healthy life with their new organs,” said R. Mark Ghobrial, MD, PhD, J.C. Walter Jr. Presidential Distinguished Chair and Director of the J.C. Walter Jr. Transplant Center. “This work brings us closer to personalized, precision therapies that could one day redefine transplantation success.”
02
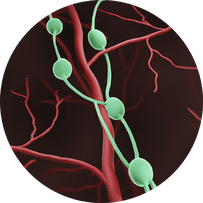
Liver Failure Avengers: Weaponizing Lymph Nodes for Battle

Meet the lymph node.
These small, bean-shaped organs found
at the convergence of major blood vessels in the body filter substances in a person’s lymph fluid. An adult has approximately 600-800 nodes located in the neck, armpit, chest, behind the ear, abdomen and groin.
Houston Methodist researchers are now in a Phase 2a Clinical Trial—Safety, Tolerability, and Efficacy of Hepatocyte Transplantation into Periduodenal Lymph Nodes Among Subjects With End-Stage Liver Disease.
Constance Mobley
MD, PhD, FACS
Under the leadership of Constance Mobley, MD, PhD, FACS, researchers have successfully performed a first-in-human miniature liver hepatocyte transplant to change a patient’s lymph nodes into ectopic miniature livers. Houston Methodist is only one of two sites partnering with LyGenesis, Inc.
More than 10,000 liver transplants were performed in 2023; however, over 1,700 patients die annually while on a waitlist per the United Network for Organ Sharing.
The team dosed four patients currently on a transplant waitlist, using their lymph nodes as living bioreactors to regenerate an ectopic organ. Selected patients must have a Model for End-Stage Liver Disease score greater than 10, but less than 25 at the time they are enrolled in the study. The goal is to have a total of 12 patients for the study, which began in 2022.
Mobley’s colleague, Sunil Dacha, MD, MBBS, performs an endoscopic ultrasound to locate the lymph nodes in the periportal area. Once Dacha locates a lymph node in that area, he endoscopically injects that lymph node with the liver cells.
“The procedure is simple; however, the difficulty lies in identifying the nodes around the liver due to their size—one centimeter or less. They are not easy to find, but with meticulous examination, we’ve successfully performed these procedures,” said Dacha, Associate Professor of Clinical Medicine.
What’s so exciting about this study is that these types of studies have never been performed in patients. We are the first hospital in the world to successfully inject these cells into a human. We always hear that Houston Methodist is leading medicine; in this instance, we actually are the first in the world to accomplish this goal.
Constance M. Mobley, MD, PhD, FACS
The first stage of this study is to meet the FDA requirements of safety, tolerance and efficacy. “With our initial patient cohort, we want to ensure that their lymph nodes are functioning like livers,” said Mobley. “Our primary endpoint is safety and tolerability.” Mobley’s team monitors their patients for a year to note any changes in their baseline liver function with the hope that their liver will become healthier.
Houston Methodist is the first hospital in the world to inject these cells into a human successfully.
If this first-in-class allogeneic regenerative cell therapy obtains FDA approval, it would enable one donated liver to treat dozens of end-stage liver disease patients, which could vastly affect the organ supply and demand imbalance for patients suffering from liver failure.
“There’s such a great need for the success of this study because there aren’t enough organs for the number of patients who are in need, “Mobley emphasized. “Once we are successful in this study, the number of patients who we will be able to treat and save from liver disease will be immeasurable.”
Mobley also noted how this can be a game changer when treating patients with liver failure who may have additional underlying conditions that can be a barrier to receiving a liver transplant.
“Ultimately, my hope is that using liver cells will allow us to rescue patients who are extremely sick and can’t tolerate surgery,” Mobley said. “Theoretically, we could get so good at this that maybe patients wouldn’t need liver transplants which would be incredible.”
Update: Data and Safety Monitoring Board Approves LyGenesis’ Phase 2a Clinical Trial to Continue Dose Escalate In Novel Trial Organ Regeneration.
03
Saving Transplants Takes Front Rho

Chronic rejection of a transplanted kidney refers to degeneration in kidney function over time as the body’s immune system attacks the transplanted kidney. Around 50% of transplanted kidneys may experience chronic rejection to some degree within five years of transplant surgery.
Research shows that chronic rejection entails processes regulated by the actin cytoskeleton and the RhoA/Rock pathway. To preserve kidney function and prevent kidney transplant failure, Houston Methodist is leading two Phase 2 clinical trials, investigating the safety and efficacy of two different pharmaceuticals impacting the RhoA pathway in transplant patients.
Interstitial fibrosis (IF) is an abnormal scar tissue between the kidney tubules and tubular atrophy (TA) is a degeneration of the tubules. Both usually occur together, signifying significant and often irreversible kidney damage and are present in approximately 45% of kidney biopsies by one-year post-transplant. Even though IF/TA plays a significant role in renal graft and kidney dysfunction after transplantation, efforts at prevention—or slowing the progression—of allograft fibrosis have been unsuccessful.
Fingolimod for the Abrogation of Interstitial Fibrosis and Tubular Atrophy Following Kidney Transplantation
The first clinical trial is ongoing and investigates whether the RhoA inhibitor fingolimod (brand name Gilenya®), safely abrogates the development of IF/TA in kidney transplant recipients compared to placebo. Fingolimod binds to sphingosine 1-phosphate (S1P) receptors on immune cells, causing internalization of the receptor and decreasing downstream RhoA activation. This fingolimod-induced disruption of immune cell trafficking also indirectly impacts activation of the Akt/mTOR pathway, leading to decreased mammalian target of rapamycin (mTOR) signaling. Preliminary data strongly suggest that fingolimod inhibits chronic rejection of transplanted hearts in a murine model by inhibiting RhoA and downregulating mTOR.
Belumosudil for Abrogation of Interstitial Fibrosis and Tubular Atrophy Following Kidney Transplantation
The second clinical trial, recently initiated, investigates whether belumosudil (brand name- REZUROCK®) safely abrogrates the development of IF/TA in kidney transplant recipients compared to placebo. Belumosudil works by blocking the activity of Rho-associated coiled-coil kinase 2 (ROCK2), which contributes to the development of immune and fibrotic diseases. Evidence shows that belumosudil was effective in preventing fibrosis and chronic rejection in a murine cardiac transplantation model.
Each clinical trial is a randomized, double-blind, placebo-controlled trial in de novo kidney transplant patients to determine if the addition of either drug—on the background of standard immunosuppression—will prevent fibrosis in the kidney transplant.
We hypothesize that mitigating the fibrogenic effects of RhoA, with either belumosudil or fingolimod, will reduce structural damage in transplanted kidneys and possible subsequent transplant failure.
Ahmed Osama Gaber, MD, FACS, FAST
John F. Jr. and Carolyn Bookout Presidential Distinguished Chair in Surgery Chair
Chair, Department of Surgery
Professor of Surgery
Houston Methodist