Science in Service
of
Medicineresult
President & CEO Letter
2025 Annual Metrics
Cycle of Translation
Visionary Gifts of Hope


Introduction

Ann Kimball and John W. Johnson Center for Cellular Therapeutics at Houston Methodist

Houston Methodist Dr. Mary and Ron Neal Cancer Center

The Food & Health Alliance within the Houston Methodist Lynda K. and David M. Underwood Center for Digestive Disorders, Immunology Center and the Fondren Inflammation Collaborative

Houston Methodist Cockrell Center for Advanced Therapeutics

Paula and Joseph C. “Rusty” Walter III Translational Research Initiative

Jerold B. Katz Academy of Translational Research

Infectious Diseases Research Fund

George and Angelina Kostas Research Center for Cardiovascular Medicine

New Endowed Chairs Positions

EnMed

Center for Bioenergetics

From Discovery to Clinic


What is "Discovery to Clinic"?

Clinical Research


Houston Methodist Conducts First-Ever Study into a Challenging Situation

Can Regulating Cellular Aging Mitigate Both Cancer and Heart Disease?

Innovative Treatment for Chronic Rhinitis is Safe and Effective


Masters of Disguise: Glioblastomas Trick the Immune System by Masquerading as Reproductive Tissue
Improved Options for Patients with Severe Retinal Vascular Disease

A New FDA-Approved Treatment for Sufferers of Chronic Constipation

Houston Methodist joins the Gulf Coast Consortia

Outcomes, Quality and Healthcare Performance


New Findings on RNA Helicases May Yield New Intestinal Disease Therapy

Houston Methodist and Pennsylvania State University Collaborate on a Smartphone App That Could Revolutionize Stroke Diagnosis

New Frontiers to Improve Cardiovascular Medicine and Disease Management

Ongoing Lessons in a Pandemic

Transplants can Boost Survival Rate of Patients with Unresectable Liver Cancers

Telehealth Video Visits During the COVID-19 Pandemic – a Glimpse into the Future?

SARS-CoV-2 Induced Chronic Oxidative Stress and Endothelial Cell Inflammation May Increase Likelihood of Cardiovascular Diseases and Respiratory Failure

Restorative Medicine


Lessening Pain After Knee Replacement Surgery

Do Motor Neurons First Die in the Brain? Study Provides Clues about ALS Origins

Bringing Back Hand Function in People with Complete Spinal Cord Injury

Novel Vascular Engineering Platforms Are a Boon for Bioengineering

Ultra-high-Resolution Scanner Reveals if Knee Injury Advances to Osteoarthritis

Houston Methodist Model Demonstrates Reversal from Heart Failure State, Creating the Potential for Innovative Treatment Avenues

Precision Medicine


Rapidly Scalable, All-Inducible Neural Organoids Could Facilitate Drug Screening for Neurological Diseases

Importance of the Coronary Artery Calcium Score in Risk Assessment and Prevention of Atherosclerotic Cardiovascular Disease

COVID-19 Infection in Crucial Brain Regions May Lead To Accelerated Brain Aging

Interleukin 9 Secreting Polarized T Cells Show Potential in Solid and Liquid Tumor Treatment

The NanoLymph: Implantable. Adaptable. Anti-cancer

Science in Service
of
Medicine
From the President
2025 Annual Metrics
Cycle of Translation
result
Trailblazing New Perspectives

Pedro T. Ramirez, MD, FACOG, is dedicated to questioning the gynecological cancer treatment status quo. As Chair of the Department of Obstetrics & Gynecology, he has spent more than 25 years treating gynecologic cancer through both open and minimally invasive surgery (MIS). While open to new surgical technologies, including MIS, Ramirez is a trailblazer in conducting randomized clinical trials that challenge the efficacy of these medical advancements to ensure the best patient outcomes. His studies have influenced international standards of care and have helped shape how these surgical technologies are evaluated during development, comparative study and clinical monitoring.
01
Artificial Intelligence:
Innovation Without Evaluation
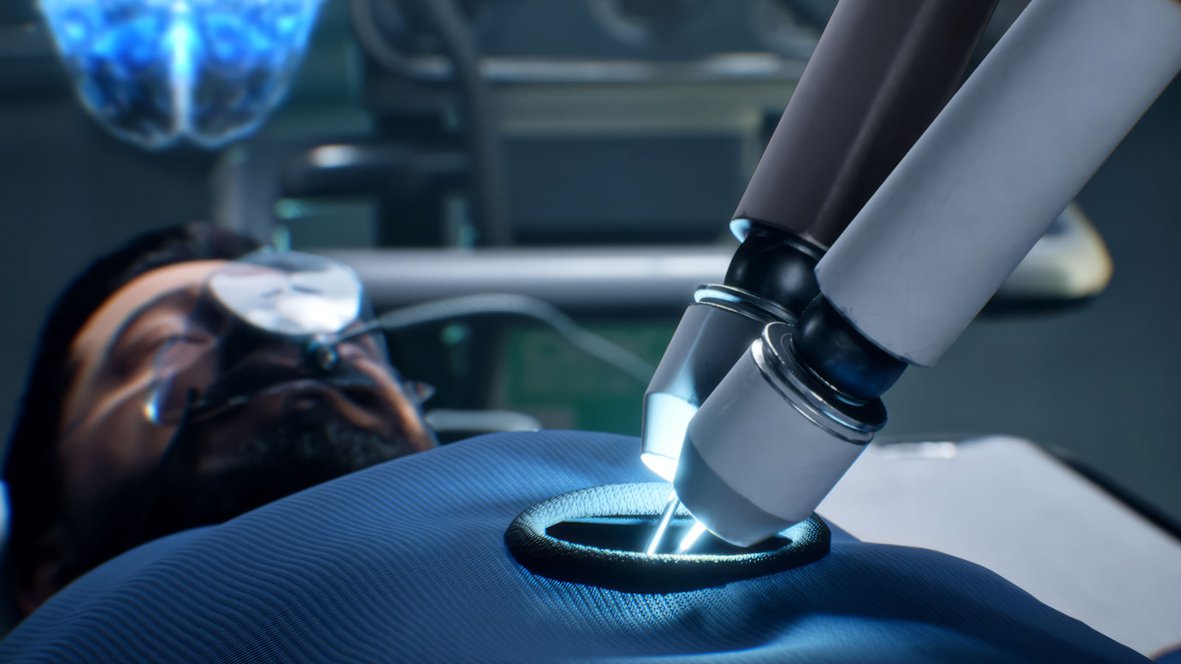
Robotic control systems and artificial intelligence (AI) programs are quickly advancing in the surgical technology landscape.

Pedro T. Ramirez
MD, FACOG
In fact, Pedro T. Ramirez, MD, FACOG, Chair of the Department of Obstetrics & Gynecology, believes that “surgical robots could perform entire procedures” in the near future. However, surgical technology, including robots and AI, are historically under-evaluated before implementation.
For most of the early 2000s, minimally invasive surgery was considered the gold-standard approach to treating cervical cancer. Then, a landmark study in 2018 led by Ramirez suggested otherwise. The study, published in the New England Journal of Medicine, revealed that minimally invasive surgery using robotics and laparoscopy to treat early-stage cervical cancer was associated with worse health outcomes when compared to the open surgery approach. These results changed the standard of care for treating cervical cancer.
Since then, Ramirez has become more involved in ensuring surgical robots are used in the safest, most effective capacity. Accomplishing this goal requires a keen focus on the continuous evaluation of surgical technology once it becomes available on the market.
“We’re moving toward a technology where the surgeon can potentially be on autopilot or standby,” Ramirez said. “These types of advancements come with ramifications if the technology is not evaluated and used properly, so, I joined the IDEAL Collaboration to help implement a robotics colloquium”
We felt that robotics needed its own evaluation framework because it is a technology that is growing so quickly and being integrated so fast. We need to become more critical of robotic technology as it is introduced to the field, especially when AI is involved and there’s potential for increasing device autonomy.
Pedro T. Ramirez, MD, FACOG
Founded at the University of Oxford, the IDEAL Collaboration is comprised of a group of research methodologists and surgeons with a common goal of improving surgical innovation research. While the group has already established an IDEAL Framework to evaluate surgical innovation and devices, the nature of surgical robots and AI pose new questions and concerns that go beyond the IDEAL Framework and the boundaries of classical evidence-based medicine.
“We felt that robotics needed its own evaluation framework because it is a technology that is growing so quickly and being integrated so fast,” Ramirez explained. “We need to become more critical of robotic technology as it is introduced to the field, especially when AI is involved and there’s potential for increasing device autonomy.”
Taking these concerns into account, in 2024 Ramirez and his team published the IDEAL Robotics Colloquium in Nature Medicine. The new framework outlines recommendations for surgical robot evaluation during development, comparative study and clinical monitoring. This framework also provides practical recommendations for developers, clinicians, patients and health care systems while considering multiple perspectives, including economics, surgical training, human factors, ethics, patient perspectives and sustainability.
02
An Open Approach for Cervical
Cancer Treatment
There’s no question that medical innovations have saved countless lives by increasing health care efficiency and efficacy, not all innovations benefit patient health outcomes compared to traditional treatment methods.
That’s why Pedro T. Ramirez, MD, FACOG, Chair of the Department of Obstetrics & Gynecology, prescribes a healthy dose of scrutiny toward such innovations.
Well-known for trailblazing the first prospective randomized clinical trial (RCT) that challenged minimally invasive surgery (MIS) as the standard of care for treating cervical cancer, Ramirez recently evaluated the feasibility of a phase three, multi-center RCT comparing the efficacy of MIS with that of the traditional open method approach (laparotomy) in treating epithelial ovarian cancer.
Published in JAMA Network Open, Ramirez explained what the feasibility study results mean for future evaluations of gynecological cancer treatment. “Currently, the open approach is considered the standard of care. If MIS shows inferior outcomes compared to the open approach, then we will have level-one evidence that MIS should not be offered as an option when performing interval cytoreductive surgery in patients with advanced ovarian cancer,” he said.
Why are health care providers scrutinizing MIS as a treatment?
Despite its wide use, there is a concerning absence of high-quality evidence supporting this surgery’s safety and effectiveness. We need to confirm that we’re not putting patients at a disadvantage by using MIS, especially given the results of my cervical cancer treatment study. As physicians and surgeons, we have a responsibility to provide treatment based on evidence-based research. I believe that the way forward in medicine is to provide a level of scrutiny that ensures the best outcomes for patients.
Pedro T. Ramirez, MD, FACOG
Final analysis of the first prospective randomized clinical trial comparing overall survival between open and minimally invasive radical hysterectomy for treating early-stage cervical cancer reveals that an open approach should be the standard of care.
The clinical trial update, published in the Journal of Clinical Oncology, reaffirms conclusions drawn from the initial 2018 publication that analyzed results at 84% lower. At the time of the initial publication, both laparotomy and minimally invasive techniques were acceptable radical hysterectomy approaches, despite limited retrospective study data evaluating survival rates of the robot-assisted surgery.
While researchers hypothesized that minimally invasive radical hysterectomy would not be inferior to laparotomy, results suggested otherwise. Of the 289 patients undergoing minimally invasive surgery and 274 undergoing open surgery, disease-free survival was 85% in the minimally invasive group and 96% in the open group at follow up (4.5 years). Overall survival was also higher in the open surgery group (96.2% vs. 90.6%), revealing a 2.5 times higher risk of death from cervical cancer in the minimally invasive group. Further, rates of recurrence of carcinomatosis were 9% in the open group versus 23% in the minimally invasive group.
“Given the higher recurrence rate and worse overall survival with minimally invasive surgery, an open approach should be the standard of care for patients undergoing radical hysterectomy for early-stage cervical cancer,” said Ramirez.
While the results were surprising to the field, there’s been significant international shifts in how cervical cancer is surgically treated.
“New technologies are exciting and may provide some benefits; it’s important to remember that evidence-based medicine should be our highest priority,” Ramirez said.