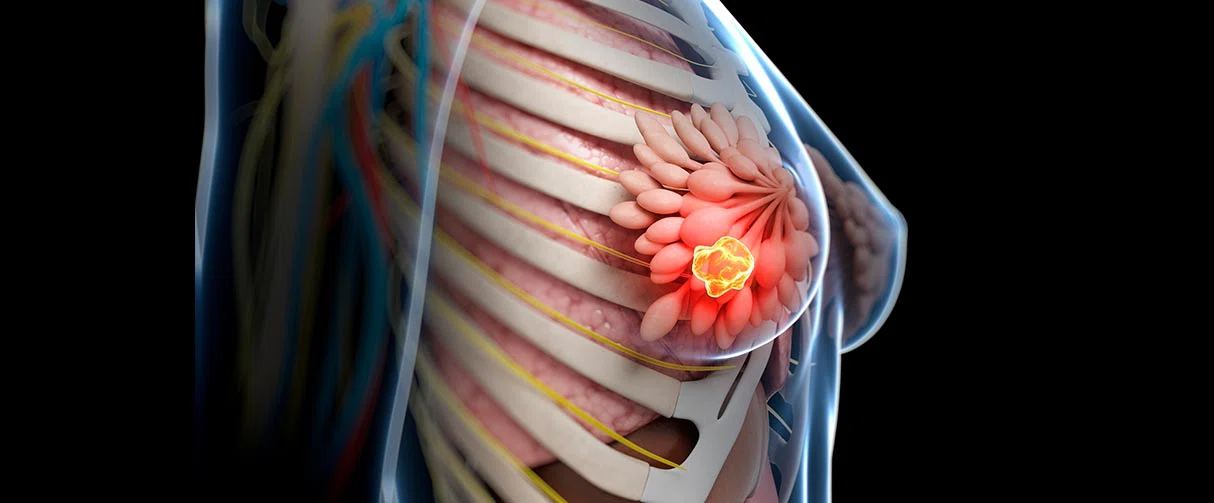
Without well-defined therapeutic targets, triple-negative breast cancer has historically lagged other cancers for sophisticated treatment strategies. However, a recently published report on a Phase I/II clinical trial conducted in Houston Methodist could offer renewed hope to patients with this aggressive form of breast cancer.
In the study, the investigators have detailed the efficacy of a novel drug combination for triple-negative breast cancer therapy that pairs, for the first time, an antimitotic medication with a nitric oxide synthase inhibitor, a drug previously studied for managing cardiogenic shock. With this formulation, the researchers reported that the patients enrolled in their study had an overall response rate of 45% with 16.7% of them achieving a complete response.
"It's an exciting new target, and it's also very non-toxic," said Jenny Chang, MD, Emily Herrmann Chair in Cancer Research and director of the Dr. Mary and Ron Neal Cancer Center. "I think this novel target has great potential for not just breast cancer therapy but also for creating a new generation of drugs for treating other cancers as well."
The therapeutic described in the journal Science Translational Medicine is patented by Houston Methodist.

I think this novel target has great potential for not just breast cancer therapy but also for creating a new generation of drugs for treating other cancers as well.


Jenny Chang, MD
Emily Herrmann Chair in Cancer Research & Director, Dr. Mary and Ron Neal Cancer Center Professor of Medicine in Oncology, Houston Methodist
While triple-negative breast cancer is relatively rare, it is more aggressive and puts patients at increased risk for metastases. Furthermore, unlike other breast cancers, the triple-negative variety holds the distinction of not expressing receptors for either estrogen, progesterone or human epidermal growth factor 2, which has impeded developing treatments tailored to the disease. And so, finding suitable biological targets for triple-negative breast cancer has been an active area of research.
Many lines of evidence from preclinical triple-negative breast cancer work have pointed to an aberrance in nitric oxide signaling. Although a tiny gaseous molecule, nitric oxide is multifaceted, playing a pivotal role in vasorelaxation, transmission and inflammation. Thus, nitric oxide is an important signaling molecule in tumor microenvironments that contain a variety of cell types, including immune and endothelial cells, alongside cancer cells.
Nitric oxide is synthesized by nitric oxide synthase enzymes, among which the inducible nitric oxide synthase and its mediated pathways have been implicated in triple-negative breast cancer metastases. Furthermore, Chang's previous in vitro work using triple-negative breast cancer xenografts in mice have demonstrated that suppressing inducible nitric oxide synthase with the inhibitor, NG-monomethyl-l-arginine (L-NMMA), decreased tumor growth and metastases.
Motivated by these results, Chang and her team conducted a Phase I/II clinical trial to test the efficacy and toxicity of different doses of the combination of taxane and L-NMMA in treating patients with metastatic and locally advanced triple-negative breast cancers. For their study, they recruited 35 patients of which 15 were for Phase I and 24 for Phase II trial.
The researchers found that the drug was well-tolerated by the patients with only 21% of patients experiencing adverse effects that were largely attributed to taxane. Further, when they analyzed the patients' serum samples for the principal metabolites of nitric oxide, nitrates and nitrites, they found a sharp reduction, pointing to a successful on-target effect of the treatment.
Patients with locally advanced breast cancer, who before the clinical trials were unresponsive to chemotherapy, were the most responsive to the treatment, having a response rate of 81% with 27% showing no residual disease at surgery. On the other hand, patients with metastatic breast cancer had a response rate of 15.4%.
Metastatic





Locally Advanced





Treatment Failure
Partial Response
Stable Disease
Progressive Disease
Complete Response
Efficacy of L-NMMA and taxane combination therapy on patients with triple-negative breast cancer
(13 metastatic; 11 locally advanced) in the Phase II trial.
Infographic designed by Sara Carr
"Chemotherapy, especially for triple-negative breast cancers, may decrease the tumor volume for a while but eventually the tumor will develop resistance," said Chang. "But by changing the tumor microenvironment, we think L-NMMA enables immune cells to once again infiltrate the tumor and have an anti-tumor, inflammatory response."
The researchers also examined circulating cytokines for a small percentage of patients and found that the immune cell milieu of patients that responded to the treatment was different from those that did not. With this information in hand, Chang said for the next stage of the study, they could do a blood test early in the treatment and based on patient immune profiles, quickly identify those that are responsive to the treatment and spare others for whom the therapy was ineffective. The researchers also plan to investigate the efficacy of their L-NMMA-based drug for different subtypes of triple-negative breast cancer.
Chang said that tweaking the formulation of a repurposed medication has helped accelerate the process of bringing their drug to clinical practice.
“The biggest hurdle in drug development is finding funding agencies that are willing to take proof-of-concept research from preclinical studies to a clinical trial," she said. "But thanks to our funding sponsors and philanthropic agencies, we did what would normally take approximately 15 years and $3 billion, in about five years while saving billions of dollars."
Andrew Chung, Kartik Anand, Ann Anselme, Alfred Chan, Nakul Gupta, Luz Venta, Mary Schwartz, Wei Qian, Yitian Xu, Licheng Zhang, John Kuhn, Tejal Patel, Angel Rodriguez, Anna Belcheva, Jorge Darcourt, Joe Ensor, Eric Bernicker, Ping-Ying Pan, Shu Hsia Chen, Delphine Lee, Polly Niravath, Jenny C Chang. A phase 1/2 clinical trial of the nitric oxide synthase inhibitor L-NMMA and taxane for treating chemoresistant triple-negative breast cancer. Science Translational Medicine (2021) 13(624): eabj5070. doi: 10.1126/scitranslmed.abj5070
This research is funded in part by the Breast Cancer Research Foundation, the Moran Foundation, Causes for a Cure, the Center for Drug Repositioning and Development Program and the philanthropic support from Dr. Mary and Ron Neal.
Vandana Suresh, PhD, February 2022
Related Articles