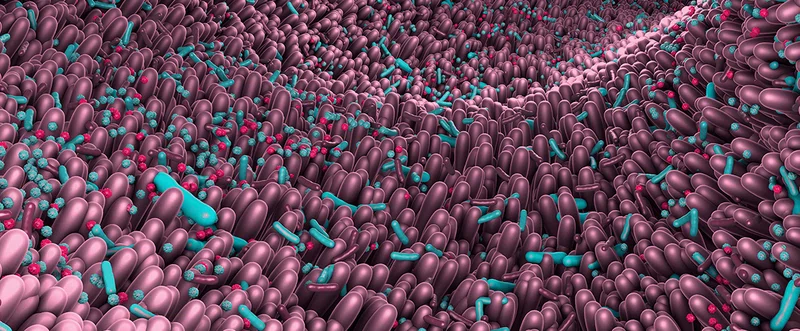
Human gut microbiota is a diverse population that plays significant roles in metabolism, nutrition, physiology and immune function. Notably, imbalance of the gut microbiota is linked to disease states such as inflammatory bowel disease (IBD), irritable bowel syndrome as well as obesity, type 2 diabetes, and atopy. The gut microbiome is also thought to offer protective immunity against colitis and colorectal cancer (CRC). However, the precise mechanisms of how microbiota contribute protective immunity in these cases are unclear. The gut microbiota, which functions in commensal, pathogenic or symbiotic relationships are composed of myriad microorganisms – the composition varying from individual to individual. Gender, ethnicity, age and diet are factors that determine the composition of human gut microbiota. This composition is thought to play a critical role in the manifestation of or protection from certain disease states.
Many of the microbiota that function in the regulation of colitis and CRC exist in commensal relationships. According to the Centers for Disease Control and Prevention, CRC is the third most common cancer type and the third leading cause of cancer-related deaths in the United States. Manifold bacterial strains associated with CRC have been identified in cancer patients and animal models. However, only a small number of bacterial strains are known to contribute protective immunity against CRC and colitis. Rongfu Wang, PhD, adjunct professor of oncology at Houston Methodist, used metagenomic sequencing to identify several bacterial taxa implicated in human Chron’s disease and cancer development and specifically identified one strain (Odoribacter splanchnicus) that confers resistance to colitis and CRC. In addition, Wang and his team produced a colitis-resistant murine model and demonstrated the cooperation of microbiota and innate immunity in regulating T helper (Th)17 cells, tissue damage and inflammation.

Although gut microbiota has been linked to cancer development and immunotherapy, little is known about specific bacterial strains that induce and modulate antitumor immunity. We identified a single bacterial strain (Odoribacter splanchnicus) that confers significant resistance to colitis and CRC through its ability to enhance key cytokine production and induce Th17 cells.

Rongfu Wang, PhD
Adjunct professor of oncology at Houston Methodist
Wang and his team developed myeloid-specific transforming growth factor-β- activated kinase-1 (Tak1)-deficient mice that are completely resistant to chemically induced colitis and CRC. This murine model is unique since most models are more sensitive to colitis as compared to wild-type controls. TAK1 is necessary for innate and adaptive immune signaling and positively regulates T cells. However, the precise function of TAK1 in microbiota, inflammation, and cancer progression is unknown. Thus, the colitis resistant model serves as a valuable resource to enhance our understanding of the mechanisms driving protective immunity against cancer and the role of microbiota.

Rongfu Wang, PhD
Adjunct professor of oncology at Houston Methodist
Intestinal microbiota interacts with the local immune system to regulate immune cell activation, tissue damage, inflammation, and cancer development. Although the consensus is to associate a mixed population of microbiota to disease progression, some specific strains of microbiota have been linked to colitis and CRC. However, few bacterial strains are known to trigger potent, protective immunity via immune modulation.
Significant differences were found in the microbiota composition of the myeloid-specific Tak1-deficient mice relative to wild-type controls. Whole shotgun metagenomics analysis was performed to identify the dominant microbiota species and strains necessary for resistance to colitis and CRC. Further screening led to the identification of the singular bacterial strain Odoribacter splanchnicus that can independently induce Th17 cells and confer resistance to colitis and CRC.
Myeloid-specific Tak1-deficient mice produce significant amounts of interleukin-1β (IL-1β), IL-6 and tumor necrosis factor-α. IL-1β and IL-6 are pro-inflammatory cytokines that contribute to inflammation-associated cancer and are required, along with other factors, for the development of Th17 cells. Th17 cells, a unique subset of CD4+ T cells, are characterized by the production of IL-17. In his recent research study published in Cell Press, Wang proposed a working model according to which myeloid-specific Tak1-deficient mice harbor unique microbiota that interact with the innate immune system to produce cytokines IL-1β and IL-6; these essential cytokines and microbiota induce Th17 cells causing Th17 expansion, which in turn, together with IL-17A, mediate resistance to colitis and CRC. Notably, intestinal Th17 cells in myeloid-specific Tak1 deficient mice were found to be necessary and sufficient to provide protective immunity against colitis.
From a therapeutic viewpoint, fecal transfer of gut microbiota may have significant benefits in reducing probabilities of tumor formation. Dr. Wang and his team discovered that the transfer of fecal microbiota from myeloid-specific Tak1 deficient mice to wild-type controls resulted in a lesser number of tumors, upon treatment with colonitis inducing chemicals. Alternately, microbiota depletion in this unique mouse model led to a conversion of the colitis-resistant phenotype to a sensitive phenotype.
According to Wang, “Although gut microbiota has been linked to cancer development and immunotherapy, little is known about specific bacterial strains that induce and modulate antitumor immunity. We identified a single bacterial strain (Odoribacter splanchnicus) that confers significant resistance to colitis and CRC through its ability to enhance key cytokine production and induce Th17 cells”.
Currently, there is a growing interest in the potential of fecal microbiota transplantation (FMT) owing to the low cost of implementation and perception of the naturality of treatment. FMT may have therapeutic potential in several conditions such as obesity, IBD, and gastrointestinal disorders. Microbiota has increasingly become key immune modulatory agents for cancer immunotherapy. Further investigation of the therapeutic potential of FMT and gut microbiota manipulation in the context of offering protective and therapeutic immunity against colitis and CRC is expected to accelerate in the near future.
Changsheng Xing, Mingjun Wang, Adebusola A Ajibade, Peng Tan, Chuntang Fu, Lang Chen, Motao Zhu, Zhao-Zhe Hao, Junjun Chu, Xiao Yu, Bingnan Yin, Jiahui Zhu, Wan-Jou Shen, Tianhao Duan, Helen Y Wang, Rong-Fu Wang. Microbiota regulate innate immune signaling and protective immunity against cancer. Cell Host Microbe. 2021 Jun 9;29(6):959-974.e7. doi: 10.1016/j.chom.2021.03.016. Epub 2021 Apr 23.
This work was in part supported by grants from the NCI, NIH (R01CA101795 and 1U54CA210181-01), and Department of Defense (DoD) CDMRP BCRP (BC151081).
Abanti Chattopadhyay, PhD, October 2021