

Archives
Face-to-Face
discover the newsletter



June 2024
Department of Otolaryngology – Head and Neck Surgery Newsletter
A Letter from the Chair
Best Practices:
Keep the Main Thing the Main Thing
Perhaps the most important job in medical academia today is to stay current with best practices. We hear the term “best practices” every day. We think it. We see it being performed. We certainly read about it. But has the concept itself become such a part of the backdrop of everything we do that we aren’t really paying attention?
No one wants to be stuck in old information, using dated techniques, relying on yesterday’s technology. Yet, we can certainly get overwhelmed by the information that is exploding exponentially around us. Technology is improving every day and moving equally fast. Now comes AI (artificial intelligence) on the scene, and we have a new source that may purport to know more about “best practices” than we do.
Mas Takashima, MD, FACS
Sylvia and James E. Norton
Distinguished New Century Chair
Professor and Chair
Department of Otolaryngology
– Head and Neck Surgery
Houston Methodist Academic Institute
Let’s start with the basics. Why are best practices in medicine critically important? The first reason is simple: patient safety. We create and recommend best practices to prevent medical errors, reduce complications, and thus reduce the length of hospital stay. Evidence-based research and clinical experience will guide us to do what’s right and safeguard the patient’s health.
Best practices create better treatment outcomes. We should never redevelop the wheel. Adhere to best practices, and patients typically will receive the most efficient and best care possible. Following best practices will lead to better disease management, quicker recoveries, and reduced mortalities. These guidelines do just that—they help guide clinicians to make the best clinical decisions with their patients.
Best practices help standardize care. A standardized approach to treating otolaryngology-head and neck surgery issues should be used across healthcare providers, from academia to private practice to residents who are trying to learn. Medicine is not static so we must facilitate continuous improvement. New evidence and new technologies are always on the horizon. We should be in a continuously improving cycle of learning and adaptation. This mindset promotes innovation; it identifies where we need to target our focus.
Also importantly, best practices or “keeping the main thing the main thing” ensure efficient use of resources. They help us avoid unnecessary tasks and unnecessary treatments that don’t add value to a patient’s care. Best practices also help us save on healthcare costs and optimize the use of available resources, keeping healthcare more sustainable. The high cost of healthcare is at the forefront of everyone’s minds these days. As the Baby Boomer bubble becomes our largest population, folks live longer and want quality lives.
Finally, best practices build credibility and trust with our patients. Patients appreciate they are receiving care that meets the highest standards based on the latest research and expert consensus. They need to know and trust us to have their care and their lives in our hands.
In academic medicine, we should take full advantage of our positions to critically evaluate peer-reviewed literature. It is an honor as well as an obligation. The number of peer-reviewed publications grows year by year, but we’re all limited in what to read. How do we know what to read? How do we process that information? In other words, how do we keep the main thing the main thing?
Two years ago, Omar Ahmed, MD, and members of our department were asked to write a best practices article evaluating the efficacy of utilizing posterior nasal nerve ablation in treating allergic rhinitis. (Is Posterior Nasal Nerve Ablation Effective in Treating Symptoms of Allergic Rhinitis? - Davies - 2022 - The Laryngoscope - Wiley Online Library)
We found that the favorable side effect profile of in-office targeted ablation of posterior nasal nerves shows a role for cryoablation or radiofrequency neurolysis in treating symptoms of allergic rhinitis.
A committee of the American Rhinologic Society also recently asked Dr. Ahmed to lead a multi-institutional panel of experts to produce an Expert Practice Statement (EPS) for posterior nasal nerve ablation for rhinitis. Our first meeting occurred at our annual Combined Otolaryngology Spring Meeting (COSM) in Chicago in May. Our plan is to publish this in IFAR (International Forum of Allergy & Rhinology), the official journal of the American Rhinologic Society and American Academy of Otolaryngic Allergy.
Our societies keep on top of what’s new, seeking out new reports and creating forums for us to discuss problems we are experiencing and ideas we are trying. If not asked to write for one of the publications, then you may have a new technique you might submit for consideration on your own. Best practices should be at the forefront of all our minds.
If you’re not constantly reading these best practices, you’re going to be practicing older or outdated medicine. I make it a point to read best practices articles most days to keep in touch with what other people are doing. Our colleagues are doing some fantastic research in various areas. I always pick up pearls of new information from these publications.
Most journals, including IFAR; Otolaryngology – Head and Neck Surgery, publication of the American Academy of Otolaryngology – Head and Neck Surgery Foundation; and JAMA (Journal of American Medical Association) Otolaryngology – Head and Neck Surgery, publication for American Head and Neck Society and American Academy of Facial Plastic and Reconstruction Surgery, Inc., include sections for “best practices.” If you don’t have time to read anything else, I recommend you read or scan through best practices.
Personally, I still like my paper journals more than online reading. In today’s age of information, I may soon need a wheelbarrow to carry my print magazines around with me. You can track our information overload by the size of these paper magazines and the way it grows month to month. It can be overwhelming.
We are setting the standards of care by putting out these articles so that other practitioners have a source they can continue to go to and learn about best practices rather than scour the volumes of literature being made available monthly and sometimes weekly. It’s the main thing. We’ve got to keep it the main thing.
ANNOUNCEMENTS
PGY1 Class Residents
Please welcome to campus our newest residents for the Department of Otolaryngology – Head and Neck Surgery.
Aatin Dhanda, MD
Rutgers New Jersey Medical School
Undergrad: Rutgers University
Kathy Le, MD
University of Texas School of Medicine at San Antonio
Undergrad: Rice University
in the news
Departmental Spotlight
Regina Jones is the calming presence who greets patients at Houston Methodist’s Center for Plastic Surgery.
READ MORE

Visiting Professor Spotlight
Gene Liu, MD, MMM, FACS, visiting professor from Cedars-Sinai Medical Center in Los Angeles, told Houston Methodist physicians in a recent Grand Rounds, “Do the right thing and rankings will come.”
READ MORE

Virtual Planning Improves Outcomes
Houston Methodist’s Head and Neck Surgery Team is experiencing better outcomes and success stories for patients with the use of virtual surgical planning to reduce times in the operating room.
READ MORE
Helping Patients Pass the Smell Test
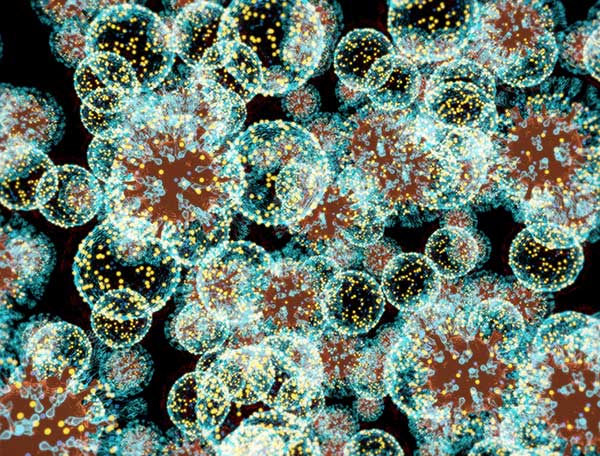
In collaboration with Cyrano Therapeutics, Houston Methodist ENT specialist Mas Takashima, MD, FACS is conducting a clinical trial to assess the efficacy of their treatment for post-viral olfactory dysfunction.
READ MORE

Feature story
Houston Methodist Doctors Return to Ukraine
As part of a long-time partnership with Canadian-based philanthropic organization, Face the Future, a team of Houston Methodist physicians recently completed their second trip to Ivano-Frankivsk in Ukraine to continue treating patients and training medical personnel in trauma care.
The Department of Otolaryngology – Head and Neck Surgery
Click here

Departmental Education
Our mission is to provide the best patient care experience while training students, residents, fellows and physician scientists
CLICK HERE

Sign up for The Department of Otolaryngology – Head and Neck Surgery newsletter
Sign up







