


clinical research
An Unusual Presentation
of Glioblastoma
Glioblastoma, or Glioblastoma multiforme (GBM), doesn’t discriminate by politics or age as we know from the deaths of John McCain and Beau Biden.
With 10,000 new cases each year in the U.S., GBM comprises 80% of primary malignant central nervous system cancers, which usually brings headaches, confusion, focal neurologic deficits, seizures, memory loss and personality changes. It’s an aggressive tumor known for its high rate of recurrence even after the most comprehensive therapy. Starting as aberrant growth of astrocytes in the brain or spinal cord, it grows quickly, invading and destroying healthy tissues.


80%
Visual loss as a manifestation of glioblastoma is well documented and can occur when the tumor invades optic pathways like the optic nerve, optic chiasm, or optic tract, compressing and damaging the delicate structures. The resulting symptoms include blurred vision, visual field defects, and in the most severe cases, complete vision loss in one or both eyes. Other neuro-ophthalmological effects such as afferent pupillary defect or optic disc edema can also occur.
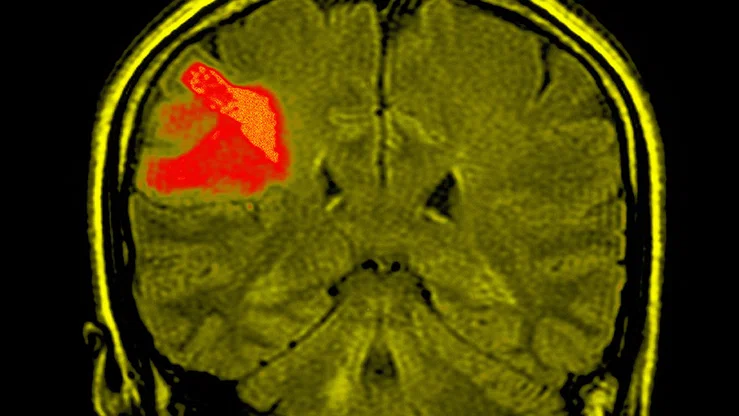
In GBM, vision loss is usually because of secondary infiltration of the posterior visual pathway. Primary involvement of the anterior visual pathway is much less common and leptomeningeal spread (LMS) of GBM is unusual. Neuro-ophthalmologist Andrew Lee, MD, Herb and Jean Lyman Centennial Chair in Ophthalmology, recently published the first-ever reported case of progressive vision loss as the presenting manifestation of recurrent GBM with secondary LMS to the optic chiasm.
At the time of this writing, there were four cases of GBM involving the optic chiasm. In none of those cases was the tumor a result of metastatic disease or LMS. Either the optic chiasm was directly invaded from glioma originating elsewhere, or it was the point of tumor origin. While some documented cases observed multiple GBM foci, the lesions were thought to be simultaneous and not due to metastasis or LMS. The case reported by Lee and his team seems to be the first description of visual loss as the presenting manifestation of LMS to the optic chiasm.

Understanding the mechanisms of T cell exhaustion remains a crucial area of research. Our findings have significant implications for advancing more potent immunotherapies that target solid tumors. Further investigations are necessary to elucidate the molecular mechanisms underlying T cell function in human cancers.

Wenhao Chen, PhD
Associate Professor, Transplant Immunology in Surgery
The patient described in the report, first presented with a primary frontal lobe GBM and progressive visual loss from chiasmal involvement of GBM due to LMS of the tumor. Initial neuroimaging showed frontal GBM without visual loss or radiographic involvement of the optic chiasm.
Approximately 30 days after a subtotal resection, the patient experienced subacute, progressive visual loss in both eyes despite postoperative chemotherapy ide and external beam radiation therapy. Upon examination, visual acuity was counting fingers in the right eye and no light perception in the left, and a left relative afferent pupillary defect. Intraocular pressure measurements, slit-lamp biomicroscopy, motility, and external examinations were normal in both eyes. Both eyes also displayed diffuse optic atrophy.
The radiation therapy could have made the patient more vulnerable to chiasmal pathology, but the extra focus of enhancement in the cauda equina outside the range of external beam radiation makes LMS of GBM involving the optic chiasm the most likely source of this visual deterioration. Caused by protease activity and expression of adhesion-migration proteins that promote GBM cell movement through the extracellular matrix, LMS occurs in up to 25% of GBM. The migration of GBM cells from the site of origin to subpial, subarachnoid, and subependymal spaces with subsequent dissemination through the CSF leads to the seeding of other sites. CSF cytology is only seen in 25%–45% of LMS of GBM cases.
The report provides guidance for physicians who may face a similarly unusual presentation of vision loss.
“Although GBM can directly involve the optic pathway, LMS presenting with visual loss in GBM is uncommon,” said Lee “Nevertheless,clinicians should be aware that rapidly progressive visual loss in GBM may be a sign of LMS.”
Cina Karimaghaei, Mohammad Pakravan, Chaow Charoenkijkajorn, Virginia A. Lee, Andrew G. Lee
Heather Lander, PhD
December 2024
Share this story
Related Articles





