


Clinical research
Could Cardioneuroablation Replace Permanent Pacemakers?
Houston Methodist Researchers Demonstrate the First Case Study in Which Cardioneuroablation Successfully Abolished Heart Block in a Patient with a Triple Orthotopic Heart Transplant
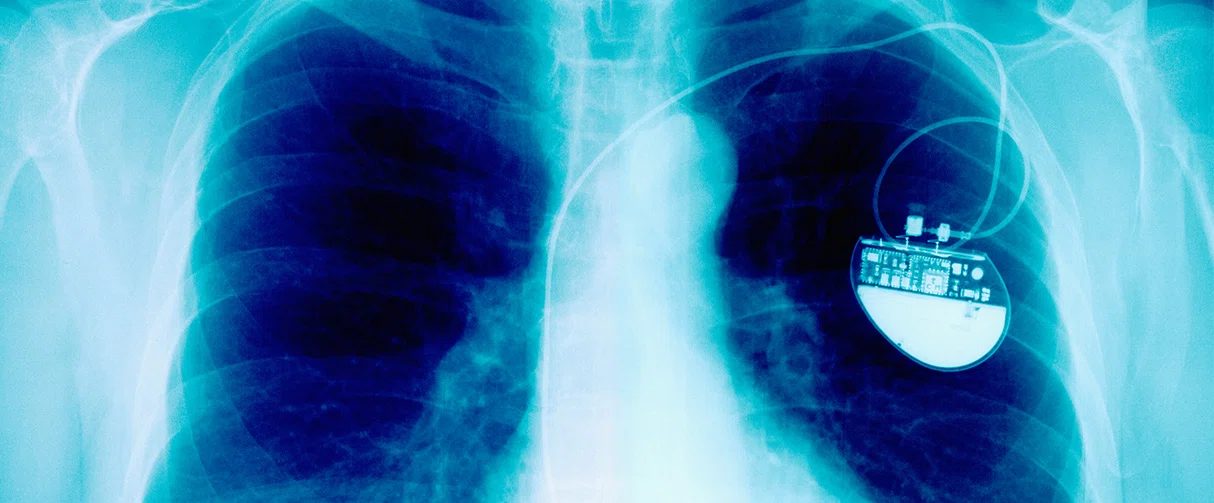
The treatment of choice for end-stage heart disease is heart transplant surgery – which can be of two types: orthotopic or heterotopic. An orthotopic heart transplant (OHT) – in which the donor’s heart is implanted post-excision of the recipient’s heart – may show several complications, including atrial and ventricular arrhythmias. Patients may exhibit sinus node dysfunction and a heart block, in which case a permanent pacemaker is the standard of care.
Miguel Valderrabano, MD, Lois and Carl Davis Centennial Chair I, DeBakey Heart & Vascular Center, professor of cardiology and program director of the Clinical Cardiac Electrophysiology Fellowship in the Department of Cardiology at Houston Methodist demonstrated the first case in which cardioneuroablation (CNA) was successfully used to abolish a high degree atrioventricular (AV) block – also known as a heart block – in a patient with triple OHT. The results of this case study, published in a research correspondence in the Journal of the American College of Cardiology: Clinical Electrophysiology in 2022 are significant since the patient was discharged without further AV blocks and showed 100% ventricular sensing with no arrhythmias or ventricular pacing at three months post-treatment. Taken together, these results indicate a conceptual breakthrough and suggest that CNA could be an alternative mode of treatment in similar cases of OHT.
Miguel Valderrabano, MD
A heart block is a partial or complete block of the electrical impulse from the atria to the ventricles – the symptoms of which can vary from none to life-threatening. A paroxysmal heart block (such as the one seen in the patient in this case study) is particularly ominous since it is characterized by a sudden appearance of a complete AV block with no escape rhythm.
The patient was a 23-year-old male with a history of triple OHT for congenital dilated cardiomyopathy. He underwent OHT in 1998 as a one-year-old, in 2018 for coronary vasculopathy, and in 2022 because of rejection. After his third OHT, the patient demonstrated a high degree AV block while asleep and underwent a dual chamber pacemaker implantation because of the perceived high risk of sudden death owing to a bradyarrhythmia (abnormally slow resting heart rate).
A normal heart beats 60-100 times per minute – which varies depending on the “state” of the individual. In an anxious setting or after strenuous exercise, the heart rate is faster as compared to a resting state. Nerve regulation of the heart rate is complex. There are nerve connections between the heart, chest and brain in a normal individual which regulate the heart rate. Due to these nerve connections, circumstances of duress or anxiety speed up the heart rate. Notably, in a newly transplanted heart, these nerve connections are absent initially.

Orthotopic heart transplant results in transection of the vagal nerve and the post-ganglionic sympathetic fibers from extrinsic sympathetic ganglia, causing complete disconnection of the graft from central connections with the central nervous system. Axonal degeneration follows, resulting in the disappearance of nerve terminals within transplanted tissue. Over time, 40% to 70% of orthotopic heart transplant recipients will reinnervate, with sympathetic reinnervation occurring five to six months postoperatively and parasympathetic reinnervation requiring one to three years. Given the perceived high risk of sudden death from bradyarrhythmia, the patient underwent dual-chamber pacemaker implantation. We suspected a neurally mediated mechanism of his paroxysmal atrioventricular block because of the absence of graft dysfunction. If high-frequency stimulation of the intrinsic cardiac nerve could replicate the atrioventricular block, we reasoned that cardioneuroablation would be therapeutic.”

Miguel Valderrabano, MD
Professor of Cardiology at Houston Methodist
A permanent pacemaker helps control a slower heart rate and long-term arrhythmias. However, the surgical procedure of implanting a pacemaker comes with several risks at the site of implantation, including infection, swelling, bruising or bleeding, blood clotting, damage to blood vessels or nerves as well as a collapsed lung. On the other hand, CNA is a simple, 30-minute procedure performed using radiofrequency catheter ablation with fewer complications.
The newly transplanted heart has functional nerve connections of its own. Interestingly, in this case study, the nerves in the newly transplanted heart were getting activated autonomously causing the heart rate to slow down. The exact mechanism behind this phenomenon is unclear, according to Valderrabano. However, this study indicates that the nerves in the heart can get activated by themselves which is a novel finding and adds insight into how the nerves in the heart function.
Created in the 1990s, the patented technique of CNA has been utilized to improve patient outcomes in cases of slower heart rates. Valderrabano has used CNA to prevent episodes of fainting in patients where this is disruptive. In this case study, however, Valderrabano cautiously explored the avenue of cauterizing nerves in a newly transplanted heart.
Click on the image above to enlarge it.
Figure 1. Mapping and Ablation of Intrinsic Cardiac Nerve by Inducing AV Block During HFS
(A) Ambulatory monitor strips showing paroxysmal high-grade atrioventricular (AV) block. (B) Biatrial 3-dimensional electroanatomic maps of the native and donor heart in right left anterior oblique projections. Black dots are sites of high-frequency stimulation (HFS) without induction of AV block. Green and fuchsia dots are sites of HFS with induction of AV block in the right atrium (RA) and left atrium (LA), respectively. (C) Response to HFS at baseline. (D) HFS response after ablation. (E) Pacemaker interrogation showing no ventricular pacing. RFA = radiofrequency ablation sites.
According to Valderrabano, “Orthotopic heart transplant results in transection of the vagal nerve and the post-ganglionic sympathetic fibers from extrinsic sympathetic ganglia, causing complete disconnection of the graft from central connections with the central nervous system. Axonal degeneration follows, resulting in the disappearance of nerve terminals within transplanted tissue. Over time, 40% to 70% of orthotopic heart transplant recipients will reinnervate, with sympathetic reinnervation occurring five to six months postoperatively and parasympathetic reinnervation requiring one to three years. Given the perceived high risk of sudden death from bradyarrhythmia, the patient underwent dual-chamber pacemaker implantation. We suspected a neurally mediated mechanism of his paroxysmal atrioventricular block because of the absence of graft dysfunction. If high-frequency stimulation of the intrinsic cardiac nerve could replicate the atrioventricular block, we reasoned that cardioneuroablation would be therapeutic”.
This interesting study underscores the possibility that CNAs may replace permanent pacemakers while offering improved outcomes for OHT recipients with heart blocks. A prospective clinical trial, albeit with a smaller sample size, may shed light on the probabilities of success that can be expected with CNA, which may aid OHT patients to make more informed decisions. More studies along these lines will help us better understand the future implications of CNA in cardiovascular medicine.
Thomas Flautt, Adi Lador, Miguel Valderrábano. Paroxysmal Heart Block After Orthotopic Heart Transplant: Evidence of Intrinsic Cardiac Nerve Activity. JACC Clin Electrophysiol. 2022 Jun;8(6):802-803. doi: 10.1016/j.jacep.2022.02.006.
Abanti Chattopadhyay, PhD
August 2023
Related Articles





