restorative medicine
What happens when the proteins maintaining brain cell health start breaking bad?
New study, for the very first time, identifies how this happens.
New study, for the very first time, identifies how this happens.
Neuronal aging can impact all areas of life, from memory to mobility.
This wouldn’t be a problem if neurons were replaced as we age, but all our neurons are produced by three to four years of age. Unlike most other human cells, neurons have very little regenerative capacity.
“Neurons are trained and learn as we grow,” said Muralidhar Hegde, PhD, Everett E. and Randee K. Bernal Centennial Chair for the Neurological Institute and Professor of Neurosurgery. “How we maintain our health impacts how they age, so most neural cells live as long as we live: maybe 80 to 90 years.”
Hegde’s team studies the molecular mechanisms of neurodegenerative diseases with a focus on genome damage and repair deficiencies in neurons. His lab is interested in neurological diseases, such as amyotrophic lateral sclerosis (ALS) and Parkinson’s disease (PD), and they’ve shown that DNA repair inhibitions/deficiencies are important in the development of such diseases.
In addition to the toll of aging, neurons are always working. Even when sleeping, neurons are busy, and their mitochondria must keep them energized to perform their critical functions. With this in mind, Hegde and his team sought to understand how mitochondrial DNA (mtDNA) damage and repair dysfunctions contribute to ALS.

Degradation of motor neurons, conceptual computer illustration.

These FUS proteins are found in normal brain cells and play a crucial role in maintaining mitochondrial health. In this study, for the very first time, we identified how it happens. Our findings unveil FUS’s critical role in mitochondrial health and mtDNA repair while offering valuable insights into the mechanisms underlying mitochondrial dysfunction in FUS-associated motor neuron disease.

Muralidhar Hegde, PhD
Everett E. and Randee K. Bernal
Centennial Chair for the Neurological Institute
Professor of Neurosurgery
Fused-in sarcoma (FUS) is a DNA/RNA binding protein involved in RNA metabolism and DNA repair. Evidence supports that FUS is associated with a variety of neurodegenerative diseases, including ALS. Traditionally, this has been attributed to the fibrillar aggregation of FUS, especially via its prion-like domains. More recently, researchers have observed a nonfibrillar self-assembling phenomenon—known as liquid–liquid phase separation—in FUS, and there’s been an increase in studies of its functions and mechanisms in neuronal health.
The team investigated the role of endogenous wildtype FUS in mtDNA repair to elucidate the mechanisms by which FUS mutations contribute to mtDNA damage and neurodegeneration. This study was published in Nature Communications and identifies critical pathways in FUS-mediated mitochondrial dysfunction.
Through a series of experiments in multiple cell lines including CRSPR/Cas9 mediated FUS knockout (KO) HEK293, Hedge’s team first established the localization and DNA repair function of FUS in mitochondria. They also looked at various disease-relevant models with FUS mutations/proteinopathy. These included ALS patient-derived cell lines with FUS mutations and their mutation-corrected isogenic control lines, autopsied ALS patient spinal cord tissues, and transgenic animal models to uncover the implications of compromised FUS functions in causing mtDNA damage and overall mitochondrial dysfunction in FUS-associated ALS.
Results showed that FUS interacts with and recruits mtDNA Ligase IIIα (mtLig3) to sites of mtDNA damage and that compromised FUS functionality hinders mtLig3’s repair role, resulting in increased mtDNA damage and mutations. They also demonstrated that rectifying FUS mutations in patient-derived cells preserves mtDNA integrity. In addition, targeted introduction of human DNA Ligase 1 (an alternative DNA repair enzyme) restored repair mechanisms and mitochondrial activity in FUS mutant cells, suggesting a putative therapeutic approach.
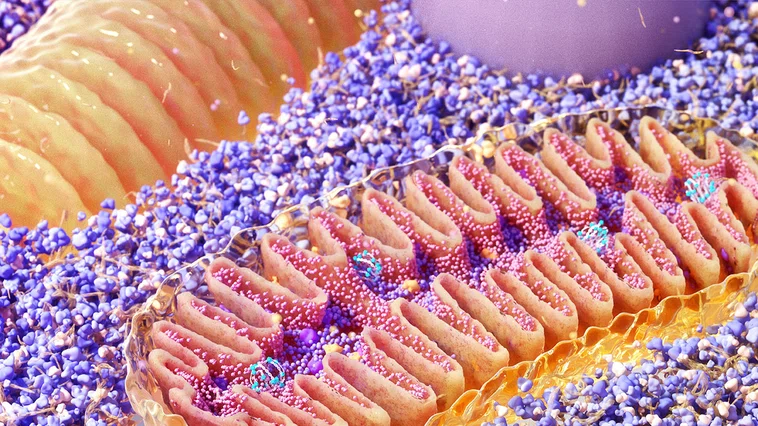
Mitochondria cross-section, illustration
“These FUS proteins are found in normal brain cells and play a crucial role in maintaining mitochondrial health. In this study, for the very first time, we identified how it happens. Our findings unveil FUS’s critical role in mitochondrial health and mtDNA repair while offering valuable insights into the mechanisms underlying mitochondrial dysfunction in FUS-associated motor neuron disease,” said Dr. Hegde.
Co-authors of the groundbreaking study include Manohar Kodavati, PhD, Dale J. Hamilton, MD, Elaine and Marvy A. Finger Distinguished Chair for Translational Research in Metabolic Disorders & Professor of Clinical Medicine at Houston Methodist, Ludo Van Den Bosch, PhD, University of Belgium, Wenting Guo, PhD, at NeuroStra Institute in France, and Alan Tomkinson, PhD, University of New Mexico. Hegde and Kodavati received the Excellence in Peer-Reviewed Publications Award from Houston Methodist Academic Institute for their work on this paper.
"The extraordinary vision, scope and impact of this research will no doubt take time to reverberate throughout the greater scientific community, but we are eagerly anticipating what new scientific insights, inquiries and innovations will follow in its wake to improve the lives of current and future generations affected by this disease," said Gavin Britz, MD, MBBCH, MPH, MBA, FAANS, Candy and Tom Knudson Distinguished Centennial Chair in Neurosurgery, Department of Neurosurgery and Professor of Neurosurgery.
Manohar Kodavati, Haibo Wang, Wenting Guo, Joy Mitra, Pavana M. Hegde, Vincent Provasek, Vikas H. Maloji Rao, Indira Vedula, Aijun Zhang, Sankar Mitra, Alan E. Tomkinson, Dale J. Hamilton, Ludo Van Den Bosch & Muralidhar L. Hegde
September 2024
Related Articles