The liver’s legendary ability to regenerate is wonderfully highlighted in the Greek mythology of Prometheus whose eternal punishment relied on the liver to regrow overnight only to be consumed by Zeus’ eagle the next day. Despite the liver’s prowess at self-renewal, certain cancers can infiltrate the liver enough to prohibit surgical resection. In these cases, transplant oncology offers patients a path toward better disease management, improved health outcomes and a potential cure.
In a review published in the journal Cancers, Maen Abdelrahim, MD, PhD, BPharm, associate professor of medicine in oncology and his collaborators have presented an overview of the evolution of transplant oncology as a treatment for certain liver cancers that cannot be surgically removed. Further, the authors have discussed the feasibility of neoadjuvant treatments before transplantation and suggest post-transplantation disease surveillance methods to optimize patient care.
According to the American Institute for Cancer Research, liver cancer is the sixth most common form of cancer worldwide with a survival rate of around 20%. The most frequently encountered form of liver cancer is hepatocellular carcinoma, which is often observed in people with cirrhosis or chronic liver disease. However, cancers inside and outside the liver are also associated with cholangiocarcinomas and the metastatic progression of neuroendocrine and colorectal cancers.

Maen Abdelrahim, MD, PhD, B Pharm
Director, Cockrell Center for Advanced Therapeutics, Associate Professor of Medicine in Oncology, Houston Methodist
Patients with liver cancer can be on long-term chemotherapy, which profoundly compromises their quality of life. Hence, when possible, cancerous tissue is surgically removed to mitigate the dependence on drug therapies. But in some instances, the authors explained, the liver is heavily scarred or has widespread cancer, making surgical resection extremely challenging. In these circumstances, liver transplantation is a line of treatment that holds promise to dramatically improve patient survival.
“Unlike for other solid organ transplants where the history of active cancer is considered as a contraindication for transplantation, liver malignancy is one of those special instances where transplantation is a viable treatment option,” said Abdelrahim.
The criteria required to screen hepatocellular carcinoma patients eligible for liver transplants were first laid by Italian physicians in 1996 and has been dubbed the Milan criteria. This selection protocol requires the tumor diameter for single lesions to be less than or equal to 5 cm, and less than or equal to 3 cm for multiple but within three lesions. In addition, the cancer must have no vascular invasion or metastasis. Liver transplants on these patients, that authors reported, boost the 5-year survival rate to 80-85%.
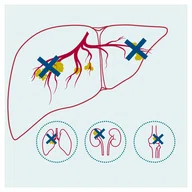
However, over the years, the Milan criteria have been expanded to include bigger liver cancers and other unresectable liver malignancies resulting from bile duct and metastatic cancers. In some cases, patients may receive bridge treatments, including chemo and immunotherapy, to downsize the liver cancer to meet the Milan criteria for transplantation.
As proof of concept for neoadjuvant bridging therapy, a collaborative effort between the Houston Methodist J.C. Walter Jr. Liver Transplant Center and Houston Methodist Dr. Mary and Ron Neal Cancer Center were the first to report a prospective case series of intrahepatic cholangiocarcinoma patients receiving chemotherapy followed by liver transplantation. These patients had a 5-year survival rate comparable to those with hepatocellular carcinoma who received liver transplants.
Milan Criteria
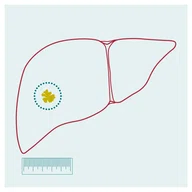
1. Single lesion ≤ 5 cm
Multiple (but within three) lesions ≤ 3 cm
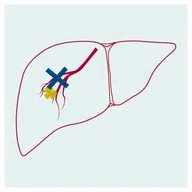
2. No vascular invasion
3. No metastasis
The authors also discussed the feasibility of minimally invasive postoperative disease surveillance methods, particularly liquid biopsies to monitor the circulating tumor DNA in the bloodstream. This technique, they said, could facilitate detecting small traces of residual disease after transplantation and propensity of disease recurrence.
Infographic designed by Rachel Whitehead
Although a promising treatment for certain unresectable liver tumors, transplant oncology is best suited for hospitals that both specialize in cancer treatment and perform transplantation surgeries at high enough volumes. Further, the field is very interdisciplinary, requiring physicians and scientists belonging to diverse disciplines, including gastroenterology, immunology and radiology, under one umbrella organization. Hence, Abdelrahim noted that Houston Methodist is one of few uniquely poised institutions to be a transplant oncology center of excellence.
“Here, at Houston Methodist, we can with our expertise grow and develop the field of transplant oncology, which is a rapidly evolving subspecialty field with very encouraging prospective outcomes,” he said.
Maen Abdelrahim, Abdullah Esmail, Ala Abudayyeh, Naoka Murakami, Ashish Saharia, Robert McMillan, David Victor, Sudha Kodali, Akshay Shetty, Joy V. Nolte Fong, Linda W. Moore, Kirk Heyne, A. Osama Gaber, Rafik Mark Ghobrial. Transplant Oncology: An Evolving Field in Cancer Care. Cancers (Basel). 2021 Sep 29;13(19):4911. doi: 10.3390/cancers13194911.
Vandana Suresh, PhD, February 2022