


Precision Medicine
The NanoLymph: Implantable. Adaptable. Anti-Cancer.
The Implantable Nanolymph Targeted Neoadjuvant Device Can Locally Recruit and Activate Antitumor Immune Cells to Elicit a Systemic Antitumor Immune Response.
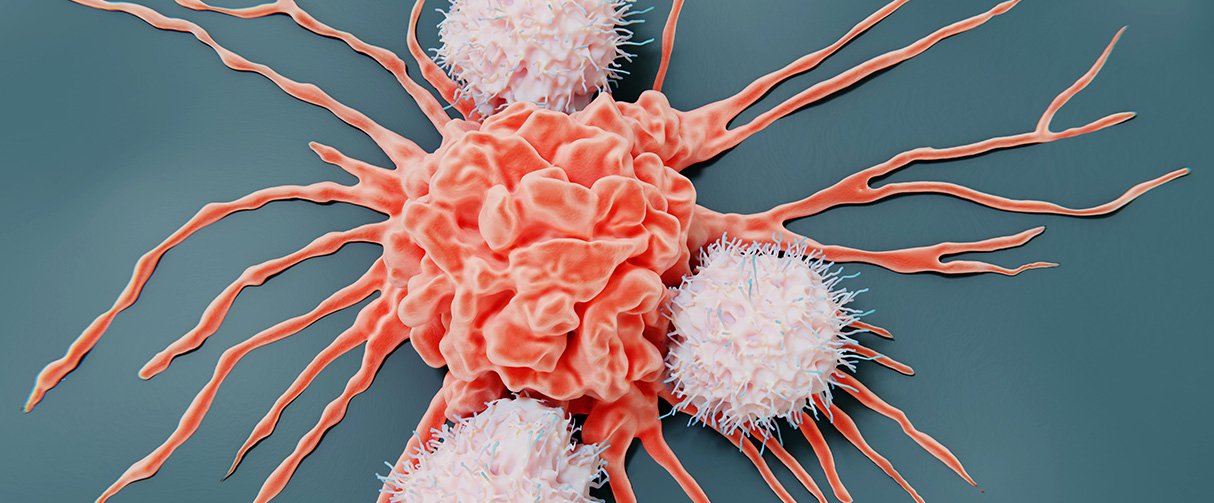
Cancer immunotherapy has revolutionized cancer treatment, but many patients don’t respond, and the approach has limited success in most solid tumors. Immunotherapy resistance can also lead to cancer relapse. Therefore, there is a critical need for boosting the response rate to cancer immunotherapy for all types of cancer and in all patient populations. And this is where targeted neoadjuvants can play a crucial role. By increasing immunogenicity and maintaining specificity, targeted neoadjuvants could be a more effective approach to eliminate tumors and evade tumor-induced immune suppression.
Alessandro Grattoni, PhD, Professor of Nanomedicine,
Houston Methodist
Corrine Chua, Ph.D.,
Assistant Professor,
Houston Methodist
Sustained and continual elution of drugs and antigens allows the NanoLymph to generate an enriched local microenvironment that is conducive to DC localization, activation and cross-presentation to T cells across the lymph system.”
Alessandro Grattoni, PhD
Professor of Nanomedicine
To be effective, targeted neoadjuvants must be able to identify tumor cells without inducing autoimmunity and must generate widespread anti-tumor immunity without systemic toxicity. Targeted neoadjuvant strategies targeting dendritic cells (DCs) – powerful antigen presenting cells – have been only minimally effective, while ex vivo strategies are prone to immune rejection and low tissue uptake with patient adherence to protocols difficult to achieve.
An alternative to previous approaches is biomaterial-based targeted neoadjuvants, which have been shown to generate antigen-specific responses that boost the cancer-immunity cascade. Several of these systems have been developed but they are limited to single administration and cannot be tailored as needed to a patient’s ongoing response to the therapy.
Rendering of NanoLymph cross-section with view of drug and antigen reservoir as well as self-sealing silicone loading ports on opposing sides. Adapted from Viswanath, D.I. et al., (2022) Engineered implantable targeted neoadjuvant platform for continuous antigen-specific immunomodulation. Biomaterials, Feb(281)
Led by Alessandro Grattoni, PhD, Professor of Nanomedicine and Corrine Chua, Ph.D., Assistant Professor, Houston Methodist researchers developed an implantable targeted neoadjuvant device called “NanoLymph” that can recruit and activate antitumor immune cells locally to elicit a systemic antitumor immune response. The device would be implanted subcutaneously and consists of a dual reservoir to hold immune stimulants and antigens. After the incision has healed and any immune response to the foreign body has resolved, the device would be loaded transcutaneously with immunostimulants and hydrogel-encapsulated antigen in the respective reservoirs. The immune stimulants would then be eluted across a nanoporous membrane into the antigen chamber forming a drug-antigen gradient within the device, which would trigger local recruitment of DCs. DCs would then interact with the encapsulated antigens in the device then head to local lymph nodes to generate a sustained systemic antitumor T cell response. Unlike other targeted neoadjuvant approaches, NanoLymph is designed to be a long-term platform that can be refilled with minimal invasiveness to provide continued immune activation that can be tailored based on a patient’s ongoing response to the therapy.
Sustained and continual elution of drugs and antigens allows the NanoLymph to generate an enriched local microenvironment that is conducive to DC localization, activation and cross-presentation to T cells across the lymph system. In addition, the authors demonstrate that the NanoLymph is biocompatible, mechanically stable and minimally invasive, making it ideal for future clinical translation.
Because of its considerable flexibility, the NanoLymph could also be utilized to effectively manage other diseases modulated by the immune system. For example, the NanoLymph could be leveraged for allergy immunotherapy to desensitize patients against common life-threatening allergens. Specifically, the NanoLymph could be used to elute cytokines or mTOR inhibitors, with house dust mite allergoid as the antigen. In this context, the NanoLymph could induce allergen desensitization by tolerogenic DCs (immuno-suppressive dendritic cells) suppressing Th2-mediated immune responses. Most available medical implants cannot be refilled and rely on either complete structure degradation or removal and reimplantation, posing a significant barrier to providing continued care.
With this publication, Grattoni and his team present a proof-of-concept study demonstrating that drug and antigen locally released from the NanoLymph in a spatiotemporal manner successfully recruits and activates DCs to induce an antigen-specific antitumor immune response. Future studies will evaluate the prophylactic and therapeutic efficacy of the antitumor immune response for cancer treatment. This work lays the foundation for development of an immunomodulatory niche that could significantly improve success of cancer immunotherapy and is also adaptable for multiple disease etiologies.
Dixita Ishani Viswanath, Hsuan-Chen Liu, Simone Capuani, Robin Shae Vander Pol, Shani Zakiya Saunders, Corrine Ying Xuan Chua, Alessandro Grattoni
Heather Lander, PhD
September 2022
Related Articles





