


outcomes research
Statin Utilization in Women
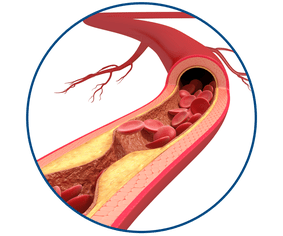
About 650,000 deaths occur each year in the U.S. due to cardiovascular diseases—a significant portion of which are atherosclerotic cardiovascular diseases (ASCVD). Caused by the accumulation of plaques inside the arterial walls, ASCVD is a major contributor to mortality and morbidity worldwide. Nearly ten percent of the adult U.S. adult population suffers from ASCVD, which includes coronary heart diseases, cerebrovascular diseases, peripheral arterial diseases and aortic atherosclerotic diseases.
Khurram Nasir, MD, MPH, Professor of Cardiology, studied a large set of adult ASCVD patients and found significant gender dissimilarities in low-density lipoprotein cholesterol (LDL-C) management using statins. Across age and racial/ethnic groups, women were found to be less likely to utilize any statins and particularly high-intensity statins. The study results, published in the American Journal of Preventive Cardiology suggest that women suffering from ASCVD are at a considerable risk of vascular events and mortality.
The plaque inside the arteries of ASCVD patients is typically composed of fat, cholesterol and other substances, and its build up leads to atherosclerosis. Growth of plaques leads to narrowing and hardening of the arteries, leading to other complications, including rupture of the plaques.

Addressing gender dissimilarities in statin use requires a multifaceted approach. Community-based approaches to increasing cardiovascular risk awareness, addressing cultural and societal biases, promoting shared decision-making, having focused campaigns on the importance of women's cardiovascular health, and increasing access to care, particularly for women with underserved and socially disadvantaged backgrounds, may help reduce the stigma around statin use. Many women may not be aware of their cardiovascular risk or benefits of statin therapy.

Khurram Nasir, MD, MPH
William A. Zoghbi, MD
Centennial Chair in Cardiovascular Health Chief
Division of Cardiovascular Prevention and Wellness
Professor, Cardiology
Cardiovascular risk assessment is therefore vital and can estimate the probability of developing a cardiovascular disease. The blood cholesterol concentration correlates with plaque formation. LDL, or “bad cholesterol,” and high-density lipoprotein (HDL), or “good cholesterol,” are the two lipoproteins that carry cholesterol to and from cells. Levels of LDL below 100 mg/dL and HDL above 50 mg/dL are considered “no risk,” whereas levels of LDL above 190 mg/dL and HDL below 40 mg/dL are considered “high risk” for ASCVD.
Statins are a class of prescription medications widely used to lower LDL levels in the blood. According to the 2018 American College of Cardiology/American Heart Association guidelines, high-intensity statin therapy is recommended for ASCVD patients 75, or younger and moderate-low intensity statins are recommended for ASCVD patients 75 or older. Since statins have a similar efficacy and pharmacodynamic profile across genders, these guidelines apply to both men and women. Notably, there are no gender-specific recommendations on statin dosing.
The study population included 98,000 adult ASCVD patients who reported to Houston Methodist Hospitals with at least one outpatient setting encounter between June 2016 and April 2022. Specifically, the study concluded that:
- despite having higher mean LDL-cholesterol (LDL-C) levels compared to men, women had 42% lower odds of using statins.
- compared with men, women were less likely to attain the guideline-defined goal of LDL-C levels of less than 70mg/dL.
- these dissimilarities were observed across age and racial/ethnic subgroups.
Zulqarnain Javed, MD, PhD, MBBS, MPH, Assistant Research Professor of Cardiology, who is an author of this publication explained, “Over the years a big focus for our department and has been the assessment of cardiovascular risk, especially through the lens of the social determinants of health and health dissimilarities. We have focused on leveraging our expertise in data science to understand and address these aspects. This study is geared towards highlighting and understanding dissimilarities in statin utilization and LDL control. In fact, this is one of the largest studies in the country to date that has assessed gender dissimilarities in standard utilization and LDL control using health system level data for over 1 million patients.”
According to Nasir and his team, the gender dissimilarities in statin utilization can be attributed to age, socioeconomic status, presence of comorbidities, patient preferences, higher rates of discontinuation and physician inertia.
However, here are some additional facts to consider:
- Statins are contraindicated during pregnancy. Hence, another contributor to the dissimilarities in statin use could be a lack of statin prescriptions from physicians in the case of women of reproductive age.
- Women are also likely to experience side-effects such as myopathy after statin use.
- Some studies suggest that women have less belief in the safety and efficacy of statins as compared to men.
- Women may prefer diet and regular exercise over statin use to reduce their ASCVD risk.
“Addressing gender dissimilarities in statin use requires a multifaceted approach. Community-based approaches to increasing cardiovascular risk awareness, addressing cultural and societal biases, promoting shared decision-making, having focused campaigns on the importance of women's cardiovascular health, and increasing access to care, particularly for women with underserved and socially disadvantaged backgrounds may help reduce the stigma around statin use,” emphasized Nasir. “Many women may not be aware of their cardiovascular risk or benefits of statin therapy.”
Women’s health, in general, is an evolving landscape. The novel insights shared in this study may lead to improvements in perceptions about medication, timely access to care for women with ASCVD risk, as well as enhanced collaboration between community stakeholders and research institutions. Furthermore, natural language processing techniques may be used to analyze unstructured clinical notes and identify patterns in physician recommendations to gather deeper insights into the observed gender dissimilarities in statin use.
“Educational and focused campaigns targeted towards women can help encourage more women with ASCVD to take statin as an adjunct therapy with adequate exercise and healthy diet. It’s also important for health care providers to involve women in the decision-making process when it comes to statin use. Further, increasing access to affordable and timely care for primary prevention of ASCVD may aid in decreasing the overall burden of this disease,” Nasir added.
Izza Shahid, Priyanka Satish, Rakesh Gullapelli, Juan C Nicholas, Zulqarnain Javed, Eleonora Avenatti, Budhaditya Bose, Shiwani Mahajan, Trisha Roy, Garima Sharma, Fatima Rodriguez, Julia Andrieni, Stephen L Jones, Sadeer Al-Kindi, Miguel Cainzos-Achirica, Khurram Nasir. Gender disparities in utilization of statins for low density lipoprotein management across the spectrum of atherosclerotic cardiovascular disease: Insights from the houston methodist cardiovascular disease learning health system registry. Am J Prev Cardiol. 2024 Aug 14:19:100722. doi: 10.1016/j.ajpc.2024.100722
Abanti Chattopadhyay, PhD
May 2025
Related Articles





