Spinocerebellar ataxias (SCAs) are a complex group of progressive neurodegenerative disorders that affect mainly the cerebellum and its afferent and efferent connections. SCAs are monogenic diseases that are primarily autosomal dominant disorders as per the nomenclature by the Human Genome Organization (HUGO). Similar ataxic disorders that show autosomal recessive inheritance are known as autosomal recessive cerebellar ataxias. In addition, there are mitochondrial, X-linked and sporadic SCA disorders that are also characterized by spinocerebellar degeneration. Collectively, the prevalence of all SCAs is 1-5.6 in every 100,000 individuals. There are less than 200,000 individuals suffering from any SCA in the United States. Hence, SCAs are characterized as rare diseases according to the criteria of the Food and Drug Administration (FDA) and the National Institute of Health (NIH).
The precise molecular events responsible for neurodegeneration in SCAs are not clear. Although a rare disease, SCA is considered a critical area of investigation by the NIH owing to three reasons. One, similarities are thought to exist between SCA and several neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s disease, Huntington’s disease and amyotrophic lateral sclerosis – for many of which the exact cause is elusive. Second, many of these disorders are known to be hereditary even though the exact genetic cause is unknown. The root cause of a genetic disorder is a mutation in a human gene; therefore, advances in SCA research (for which an increasing number of genes have been identified) can be extended to enhance our understanding of the pathogenesis of other neurodegenerative disorders. Third, treatment strategies for SCA may also be similarly extended.
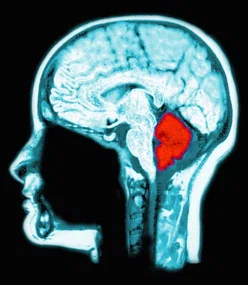
The different types of SCA are described using the prefix ‘SCA’ followed by a numeric reflecting the order of genetic discovery. Currently, 48 SCA types exist, and this number continues to grow. Typically, these are autosomal dominant ataxias with defined genetic loci. Different SCA types may have unique symptoms; the disease onset and progression patterns vary according to subtype. As the cerebellum controls movement, typical symptoms entail ataxia, uncoordinated gait, poor hand-eye coordination, slurred speech, involuntary eye movement, vision problems, learning and memory disorders and eventual loss of independence. Symptoms tend to progressively worsen and, depending on the SCA type, can appear anytime from childhood to late adulthood. However, usually disease onset is between 30 and 50 years of age.
Typically, SCAs have a high disease penetrance and dominantly inherited SCAs can be further subdivided into two categories based on the genetic mutations: SCAs caused by microsatellite repeat expansions and those caused by point mutations. The most common SCAs are repeat expansion SCAs, particularly those with polyglutamine-coding CAG repeat expansions, including SCAs 1, 2, 3/Machado-Joseph disease, 6, 7, 17 and Dentatorubro-pallidoluysian atrophy. Out of all SCAs, SCA3 is the most common. Typically, repeat expansion size determines disease severity, progression rate, age of onset and a broader spectrum of clinical symptoms. The expanded repeat sequences are also transcribed into RNA, which can be toxic. In addition, the pathology in SCA8, 10, 12, 31, 36 and 37 is caused by nucleotide repeats in non-coding regions possibly resulting in toxic RNAs.

Tetsuo Ashizawa, MDProfessor of neurology at Houston Methodist

While READISCA combines the forces of the United States and Europe, future efforts are needed to strengthen global collaboration. SCAs are a group of rare diseases, and only international cooperation can achieve sufficient sample sizes to reach enough power. An international task force with shared data will also be important to investigate how the ethnic, genetic, and/or environmental factors influence monogenetic disorders, such as SCAs.

Tetsuo Ashizawa, MD
Professor of neurology at Houston Methodist
SCAs caused by point mutations are extremely rare. These include missense mutations, deletions or duplications of DNA segments leading to a novel toxic function or a dominant-negative effect via the mutant protein. The causative gene for some SCAs has been identified. However, for many other SCA types, the genetic cause is unknown. Genetic testing and carrier testing are available for many genes known to cause SCAs. However, genetic testing is an option only when the causative gene is known. In many cases, SCA diagnosis is based on observation of typical symptoms and family history of SCA. The increasing use of the next generation sequencing (NGS) can now identify additional cases of SCA.
Although there are currently no approved treatments for SCA, recent developments in molecular biology targeting the genetic underpinnings hold promise. Several strategies are being employed to silence the toxic RNA via antisense oligonucleotides and other RNA silencing molecules. The therapeutic approaches for SCAs include inhibiting transcription, targeting the disease transcript, inactivating or reducing the mutant protein, and targeting specific downstream pathways. Editing the disease gene via Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and other gene-editing technologies is an attractive treatment that corrects the root cause of genetic diseases such as SCAs.
Clinical trials with promising therapies are another significant step towards identifying therapeutics and can convey invaluable information to enhance the quality of life of SCA patients. However, since SCA is a rare disease, several challenges exist including obtaining large cohort sizes and having sensitive biomarkers and clinical outcome assessments (COAs). This underscores the importance of international and global collaborations amongst ataxia researchers.
Various strides have been accomplished since the inception of collaboration between ataxia research networks. The Clinical Research Consortium for Spinocerebellar Ataxias (CRC-SCA) is a noteworthy natural history study that focused on various COAs and SCA genetic modifiers. In 2017, the CRC-SCA initiated an NIH-funded, 5-year longitudinal study called Clinical Trial Readiness for SCA1 and SCA3 (READISCA) which was the first US-European collaborative SCA project.
Tetsuo Ashizawa, MD, the Harriet and Joe B. Foster Distinguished Chair in Neurosciences and professor in the, Stanley H. Appel Department of Neurology at Houston Methodist, is currently studying neurogenetic disorders caused by expansions of DNA sequences that are connected end-to-end and abnormally repeated, including SCAs as well as myotonic dystrophies, Friedreich’s ataxia and Huntington’s disease. In his recent publication in Frontiers in Neurology, Ashizawa highlights the importance of global collaboration amongst researchers in order to gather a range of insights and obtain a sample size large enough to obtain statistical power within the clinical trial design.
According to Ashizawa, “While READISCA combines the forces of the United States and Europe, future efforts are needed to strengthen global collaboration. SCAs are a group of rare diseases, and only international cooperation can achieve sufficient sample sizes to reach enough power. An international task force with shared data will also be important to investigate how the ethnic, genetic, and/or environmental factors influence monogenetic disorders, such as SCAs.”
Various innovative strategies are being developed to identify potential SCA therapeutics. Clinical trials using RNA silencing technologies are set to commence in 2022. In addition, the CRISPR/Cas9 system has been successfully used to delete expanded CAG repeats in induced pluripotent stem cells. We expect the CRISPR/Cas9 system to have applications in the future. Although hurdles still exist within the realm of SCA clinical research, we are establishing clinical trial readiness with the hope of finding therapeutic and neuroprotective agents that will elevate the quality of life of SCA patients.
For further information on Ashizawa’s work on this topic please see the following papers:
Chih-Chun Lin, Tetsuo Ashizawa, Sheng-Han Kuo. Collaborative Efforts for Spinocerebellar Ataxia Research in the United States: CRC-SCA and READISCA. Front Neurol 2020 Aug 26;11:902. doi: 10.3389/fneur.2020.00902. eCollection 2020
Tetsuo Ashizawa, Gülin Öz, Henry L Paulson. Spinocerebellar ataxias: prospects and challenges for therapy development. Nat Rev Neurol. 2018 Oct;14(10):590-605. doi: 10.1038/s41582-018-0051-6
Katia M Konno, Marise Bueno Zonta, Ana T B Guimarães, Carlos Henrique F Camargo, Renato Puppi Munhoz, Salmo Raskin, Tetsuo Ashizawa, Helio A G Teive. Balance and physical functioning in Spinocerebellar ataxias 3 and 10. Acta Neurol Scand. 2021 Apr;143(4):458-463. doi: 10.1111/ane.13384. Epub 2020 Dec 10
Linliu Peng, Shang Wang, Zhao Chen, Yun Peng, Chunrong Wang, Zhe Long, Huirong Peng, Yuting Shi, Xuan Hou, Lijing Lei, Linlin Wan, Mingjie Liu, Guangdong Zou, Lu Shen, Kun Xia, Rong Qiu, Beisha Tang, Tetsuo Ashizawa, Thomas Klockgether, Hong Jiang. Blood Neurofilament Light Chain in Genetic Ataxia: A Meta-Analysis. Mov Disord. 2021 Sep 14. doi: 10.1002/mds.28783
Abanti Chattopadhyay, PhD, December 2021