Precision medicine
The power of nanotechnology to manipulate theranostics and technology in cardiovascular disease management

Cardiovascular diseases (CVD) account for countless deaths globally and one in four in the United States. The leading cause of death in the United States according to the Centers for Disease Control and Prevention, CVDs are increasing precariously although many of the risk factors are avoidable, including sedentary lifestyles, alcohol use, tobacco use, and diets high in trans-fat, saturated fat, and cholesterol. High blood pressure or hypertension, the leading contributing CVD risk factor, is clinically asymptomatic and often undetected, leading to a delay in treatment.
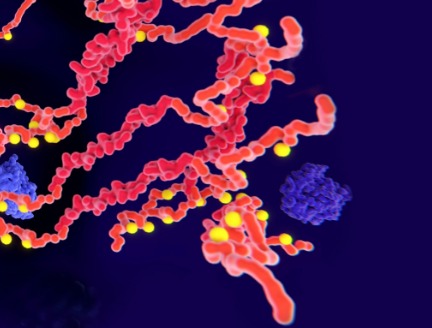
The majority of CVD treatments include oral medications and invasive surgery. Conventional drug administration for CVD management entails instability, poor bioavailability, poor solubility, poor absorptions and undesirable side effects. Nanomedicine is an attractive system that can bypass many of these issues and deliver drugs to the targeted vessels to treat CVDs such as atherosclerosis, hypertension, myocardial infarction and thrombosis.

Carly S. Filgueria, PhD
Associate professor of Nanomedicine
at Houston Methodist
Nanotechnology for CVDs has concocted nanocarriers that consist of a nanoparticle core, therapeutic payload, and targeting moiety for controlled delivery to the cardiovascular system while bypassing complex biological barriers. Recent advances in cardiovascular nanomedicine additionally encompass biosensors, actuators and wearable cardiac monitors that aid in the diagnosis, prevention and management of CVDs. In a recent perspective article published in Nanomedicine, Carly S. Filgueira, PhD, assistant professor at the Houston Methodist Department of Nanomedicine and Cardiovascular Surgery details the current practices in cardiovascular nanomedicine as well as future directions such as nanotechnological inclusions, nanocomposites, and nanocoatings.
Cardiovascular nanomedicine employs many therapeutic strategies that include targeting inflammation, thrombosis, and angiogenesis. A notable example is the vitronectin receptor, which is a marker for active angiogenesis. By targeting the vitronectin receptor, nanoparticles offer anti-angiogenesis therapy via delivery of anti-angiogenic drugs. Interestingly, nanoparticles can also be used for visualization with magnetic resonance molecular imaging made possible via intramural binding at sites where stent placement is not feasible. Moreover, because of advances in nanotechnology, therapeutics can now be delivered to the heart through intramyocardial, intrapericardial as well as intravenous injections.
With the unique ability to precisely manipulate structure at the nanoscale, nanotechnology could play a major role in device improvements and sensitivity as well as in targeted, controlled therapeutic delivery. With the unique ability to precisely manipulate structure at the nanoscale, nanotechnology could play a major role in device improvements and sensitivity. CVDs are estimated to be the most expensive condition to care for, but by generating technologies and devices that are proven to prevent and treat adverse cardiovascular events and making them accessible to all, we can increase the quality and years of healthy life while also eliminating the health disparities associated with CVD.”

Carly S. Filgueria, PhD
Associate professor of Nanomedicine at Houston Methodist
Filgueira describes nano-drug carriers, nanocarrier vascular targets, nanocarrier cardiac targets, and futuristic nanotechnological applications. The main domain of cardiovascular medicine is payload delivery via a nanocarrier. Nano-drug carriers function in diagnostics as well as delivery of therapeutics to the site of CVD. Some examples include liposomes, lipoproteins, copolymers, and dendrimers. Each has individual pros and cons.
Liposomes can be ligand conjugated or combined with antibodies against cell adhesion molecules and chemokines to target atherosclerotic lesions. Interestingly, liposomes can also be utilized for drug delivery in treating strokes owing to their ability to cross the blood-brain barrier. This attribute, along with their low immunogenicity, makes liposomes commendable nano-drug carriers. However, they lack long-term stability which is associated with premature drug release, heavy cost burden and complications with scaling up.
On the other hand, lipoproteins are non-immunogenic and naturally attracted to some disease sites because of which they can bypass immunological responses even while carrying amphiphilic and hydrophobic drugs. Moreover, lipoproteins do not need additional conjugation steps as they already possess surface components for selective cell targeting – making them superior to liposomes.
Copolymers are useful in treating cardiovascular inflammatory diseases because of their ability to deliver stem cells, proteins, small interfering RNAs and microRNAs. Another applicable category is that of highly branched polymers called dendrimers, which prevent thrombosis and deliver poorly soluble agents such as hormone mimetics. Aside from their toxicity, dendrimers offer several advantages over other nano-carriers owing to their low polydispersity, low leakage, high solubility, high stability, and low immunogenicity.
Apart from payload delivery and tunable drug release, nanotechnology has revealed several breakthroughs in the medical device space encompassing diagnosis (via improved sensors), continual symptom monitoring and remote-controlled manipulation to aid in disease prevention and repair. For instance, wearable devices or smartphone-based applications allow monitoring of heart rate and arrhythmias via artificial intelligence algorithms in high-risk CVD patients.
It should be noted that many contemporary cardiovascular nanomedical approaches were primarily exploited in targeted cancer therapy. In the near future, enhanced communication between electronics and biological systems using engineered nanoparticles and nanofluidic devices might be in practice. Silver nanoparticle-based coatings, strikingly, could leverage the human body’s tolerance to silver to release antibacterial agents without causing systemic toxicity.
According to Filgueira, “With the unique ability to precisely manipulate structure at the nanoscale, nanotechnology could play a major role in device improvements and sensitivity as well as in targeted, controlled therapeutic delivery. With the unique ability to precisely manipulate structure at the nanoscale, nanotechnology could play a major role in device improvements and sensitivity. CVDs are estimated to be the most expensive condition to care for, but by generating technologies and devices that are proven to prevent and treat adverse cardiovascular events and making them accessible to all, we can increase the quality and years of healthy life while also eliminating the health disparities associated with CVD.”
Nanocarriers have a compelling presence in modern medicine and disease treatment because of their suitability and versatility in drug delivery to disease sites while circumventing biological barriers. In the context of CVD treatment, nanotechnology has unique applications – both in drug delivery and the usage of sensors and detectors. This growing field of nanotechnology offers a unique opportunity to reduce the CVD burden and the silent CVD epidemic, while simultaneously advancing CVD management by critically monitoring risk factors to prevent early disease onset.
Dennis K Wang, Maham Rahimi, Carly S Filgueira. Nanotechnology applications for cardiovascular disease treatment: Current and future perspectives. Nanomedicine 2021 Jun;34:102387. doi: 10.1016/j.nano.2021.102387. Epub 2021 Mar 20.
This work was made possible in part by the generous support of the George and Angelina Kostas Research Center for Cardiovascular Medicine and the Houston Methodist Research Institute.
Abanti Chattopadhyay, PhD, September 2021