Restorative Medicine
New Procedure May Rapidly Restore Function in Severed Facial Nerves
Clinical trial underway at Houston Methodist tests efficacy of polyethylene glycol nerve fusion technique in rejoining transected facial nerves.

With its long reach and many intricate branches, the facial nerve envelops many of the muscles in the head and neck. Thus, damage to this vital nerve has dire repercussions that go beyond the inability to smile or convey a look of suspicion with a furrowed brow. Facial nerve paralysis or weakness can lead to a whole range of difficulties, from slurred speech to problems with eating and drinking.
As a therapeutic intervention, an upcoming treatment called polyethylene glycol or PEG nerve fusion might offer a better standard of care to rejoin severed nerves. In a Phase II clinical trial at Houston Methodist, a team of physicians is currently testing the safety of a PEG fusion surgical product NTX-001 in connecting mechanically separated nerves in the face. The study is led by Michael Klebuc, MD, associate professor of clinical plastic surgery.

Michael Klebuc, MD
Associate Professor of
Clinical Plastic Surgery at
Houston Methodist
“This procedure is one of the most exciting things in peripheral nerve surgery in the last 75 years,” said Klebuc. “PEG nerve fusion may potentially allow us to connect the facial nerves back together and immediately restore functionality.”
The facial nerve is the seventh cranial nerve and originates out of a part of the brain called the pons. It has sensory, motor and parasympathetic functions. Thus, in addition to allowing movements and sensations in the face and neck, the nerve also controls glands, such as those that produce tears and saliva. An injury to the facial nerve, such as from illnesses or injuries, can lead to the loss of a multitude of functions and profoundly affect an individual’s quality of life.
Unlike the nerves of the central nervous system, those in the periphery, including the facial nerve, can regrow. The complex biochemical process begins within minutes after an injury and is modulated in part by calcium. Put simply, an increase in calcium levels within the nerve fiber after a trauma causes vesicles, or biological cargo-carrying pockets, within the axon to release their contents. These molecules then plug the holes in the membrane, capping off the healthy end of the nerve fiber from damaged portions downstream.
Over the course of days, in a complex process called Wallerian degeneration, the damaged portions of the nerve fiber are broken down and cleaned up by the immune system. It is only after the removal of this debris that the nerve begins to slowly grow toward the muscle.
“The regeneration of a transected nerve is very gradual, at about a millimeter a day or an inch a month. So, it can take a very long time for the nerve to reach its target,” said Klebuc. “By the time it gets there, there's usually muscle atrophy, which leads to permanent weakness, and the regenerative process is never 100%.”
This limitation, he said, may be overcome with the PEG nerve fusion technique. The PEG fusion product prevents Wallerian degeneration and nerve capping, thereby making nerves more conducive to fusing. The success of PEG nerve fusion in preclinical studies has launched human clinical trials that are currently evaluating PEG nerve fusion to rejoin peripheral nerves in the body’s upper extremity. Joining these efforts, Houston Methodist is a recruiting site for testing PEG nerve fusion product NTX-001 for severed facial nerves.
Shown is a free gracilis muscle flap. PEG nerve fusion can speed up the innervation of a motor nerve branch (yellow) from the masseter muscle. Image courtesy Michael Klebuc, MD.
Participants in the study include those who have had a cut in their facial nerve within 48 hours, and the transected region excludes the intracranial portion of the nerve. Most patients with Bell’s palsy, Ramsay Hunt Syndrome or infection-caused nerve damage are not included; in these cases, the nerves can have a mix of injuries and could be partially recovered. Additionally, individuals unable to adhere to the postoperative monitoring protocol were excluded.
Although the study is still ongoing, Klebuc said the technology has great promise.
“With the PEG nerve fusion, the nerves start to function within about three minutes of fusing,” he said. “It’s pretty amazing. If someone cuts their cheeks and can’t move their face at all, you could take them to the operating room, join the nerves back together with PEG and then, in the recovery room, they could be moving their face.”
PEG nerve fusion, Klebuc noted, would also be extremely useful when a nerve needs to be rejoined after it is transected to remove a tumor of the parotid gland, for instance. Another scenario for the PEG nerve fusion to restore facial movements is in patients after a brain tumor is removed. In these individuals, a portion of the gracilis muscle in the thigh along with its nerve and blood vessels are transplanted to the face. Typically, a branch of the nerve that facilitates chewing is then allowed to grow into the transplanted muscle, a process that takes months. But with PEG fusion, that nerve could be directly fused to the nerve endings coming from transplanted muscle.
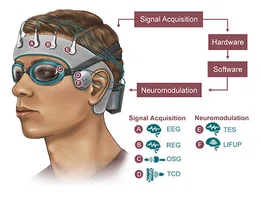
As the trial progresses, Klebuc and his team are also looking for innovative ways of quantifying the outcomes of patients receiving the PEG nerve fusion.
“We're evaluating patients with some pretty interesting technology to make better assessments of the success of nerve fusion,” said Klebuc. “We're using cutting-edge facial recognition and video technologies to make measurements of the nerve before and after the intervention, and we'll be able to see facial motion changes down to the millimeter.”
Vandana Suresh, PhD
November 2022
Related Articles