

Archives
Patient-driven network emerges from daunting nose reconstruction
A peer-driven support group at Houston Methodist Hospital has become central to easing the emotional and physical journey for patients undergoing nose reconstruction following skin cancer. Anthony Brissett, MD, FACS, one of the nation’s leading facial plastic and reconstruction surgeons, says a "patients-helping-patients" community emerged organically from his patients who wanted to build relationships with others who were undergoing daunting forehead-flap procedures.
“We have a small army of people who supported each other while they learned about the process, continued to help each other through an extensive reconstruction period, and now keep in touch,” Dr. Brissett said. “Some of these procedures can be extensive. As a result, there’s a lot of misgivings that go along with recovery and results,” he said.
He credits patient Amy Leach of Midland, Texas, as the lynchpin of this patient network that was sparked when she voluntarily offered her contact information to support others experiencing similar procedures. Amy’s surgery was in 2017, and she continues to offer her encouragement to others eight years later.
“We now have our own ecosystem that builds on Amy’s foundation,” said Dr. Brissett, professor and vice chair of Houston Methodist Hospital’s Department of Otolaryngology – Head and Neck Surgery and division chief of Facial Plastic and Reconstructive Surgery. Dr. Brissett also recently was installed as President of The American Academy of Facial Plastic and Reconstructive Surgery.
Facial Skin Cancers
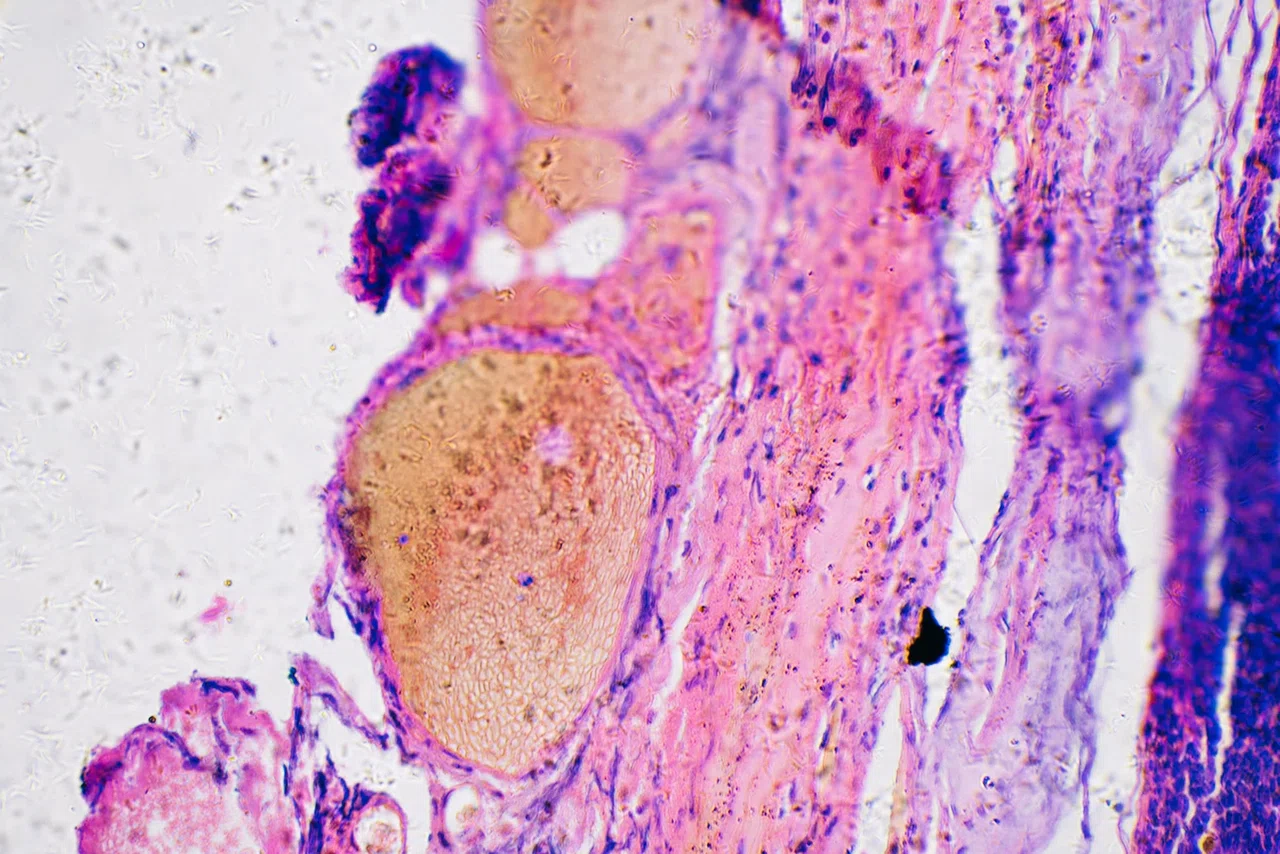
Nose skin cancers account for 30 percent of all facial skin cancers and often require complex, multi-stage surgeries that can be emotionally and physically difficult. Even more overwhelming is the recovery process in between procedures when skin from the patient’s forehead or scalp temporarily create a “flap” of healthy, growing skin that eventually will be used to recreate the nose. Some patients choose to stay home during the interim when their nose is being reshaped. They can find themselves housebound too long and depressed.
Amy said she was hoping for an easy outcome from her nose surgery but, in the process, began to pray instead, ‘Lord, please use my circumstances to encourage others, and He certainly did and continues to do so,” she said. “I thought I wouldn’t come out of my house for six weeks, but I realized there might be others who would benefit from my experience,” she said.
Amy and others of Dr. Brissett patients openly share their nose cancer journeys and offer reassurance to new patients facing the procedure. Patients often need a touchstone to keep them hopeful.
“I think the reason I did not have much depression during the three months I stayed home was because of the relationship I had with Amy,” said Jimmie Sue Siptak, a
retired school counselor. Jimmie Sue’s surgery was also in 2017 but took place a few months after Amy already had gone through the procedures and recovery.
“Amy provided a community for me. She encouraged me, shared with me, and often was able to answer questions and concerns I had,” Jimmie Sue said. “She was a little bit down the road after her procedure, so I could see her results were beautiful.”
Jimmie Sue said she was “blindsided” when Dr. Brissett told her what to expect, but Amy was in the waiting room ready to speak to her. “She treated me like family, and that’s what I really needed – someone to really care about me and knew what I was going through.”
Patient Sherri Lowe, of New Braunfels, also described the struggle and hope that comes with the process. “The anticipation and learning about everything I needed to know was far more suffering than the actual experience of the surgery and recovery,” said Sherri, who underwent reconstruction after Mohs surgery in 2022.
Amy and Sherri met face to face when they happened to be scheduled at the dermatologist/Mohs surgeon’s office on the same day. Amy was there for her regular skin checkup while Sherri was there for her initial Mohs surgery to remove the cancer.
After having had many conversations over the phone, it was so sweet of God to orchestrate our appointments on the same day. I was so pleased to sit with Sherri in the patient room and pray with her while we waited.
Amy Leach
From left, Dr. Brissett, and patient network Sherri Lowe, Amy Leach and Jimmie Sue Siptak
“It was like we knew each other forever,” Sherri added. “Our journeys aligned in many ways. Amy’s kindness reminded me to accept help from others — something that isn’t easy for me because I am used to always being the carer. It was because of Amy that I was led to believe I could do what she did.”
Bambi Saporito of The Woodlands lived in Houston when Sherri was in town for a checkup with Dr. Brissett. “I was living a mile from the medical center, and Sherri said, ‘just stay there and I’ll come to you.’ She looked so great that it gave me hope.
“I am so grateful to Sherri and Amy,” Bambi said. “They made such a huge difference. These ladies didn’t just come and talk; they came with bags of goodies. They brought things I wouldn’t have even thought of,” she said.
“There were places where I would’ve turned around and been happy to run away. But these two ladies kept sending me all the scripture I needed to hear, saying ‘you’ve got no control. You’ve got to trust Him, put one foot in front of the other and take yourself to the hospital,” Bambi added.
Experts at Houston Methodist’s Department of Otolaryngology – Head and Neck Surgery are working to create awareness within the institution and with dermatologists and Mohs surgery specialists in the community to provide a comprehensive skin cancer program. This includes work with Houston Methodist’s multidisciplinary tumor board to discuss and determine current and best cancer treatments and follow-up reconstructive surgery.
Dr. Brissett emphasized the importance of peer support for surgeries that can appear disfiguring for a while during recovery. “Having a group that’s gone through it can be very supportive. In the midst of this storm, these patients have created a powerful aspect of my practice.”
Facial Skin Cancers
Nose skin cancers account for 30 percent of all facial skin cancers and often require complex, multi-stage surgeries that can be emotionally and physically difficult. Even more overwhelming is the recovery process in between procedures when skin from the patient’s forehead or scalp temporarily create a “flap” of healthy, growing skin that eventually will be used to recreate the nose. Some patients choose to stay home during the interim when their nose is being reshaped. They can find themselves housebound too long and depressed.





