


Otolaryngology OR is a vision of the future
Otolaryngology OR is a vision of the future
When visiting physicians and professors come to Houston Methodist Hospital, they say they feel like they are stepping into the future of surgical care for Otolaryngology, Head and Neck Surgery.
“This is like looking at something that one dreams about but could never quite attain. Here it is in the flesh and working as intended,” said Professor Peter John Wormald, Chairman Of Otolaryngology, Head and Neck Surgery at the University of Adelaide in Australia.
Dr. Wormald, one of the world’s top sinus surgeons and a recognized leader in sinus-related technology, recently visited Houston Methodist to tour the specialized operating room (OPC 18) for otolaryngology. He also visited Houston Methodist Institute for Technology, Innovation and Education (MITIE), Methodist’s virtual hospital and hands-on clinical training facility as well as other faculty members and specializations of the Department.
“The Methodist Hospital ENT group is not only reaching for the stars, but they are almost there,” Dr. Wormald adds. He said the communications set up between facilities and the conference room bring “amazing” levels of technology.

Professor Peter John Wormald, Chairman Of Otolaryngology, Head and Neck Surgery at the University of Adelaide in Australia
“Technology here is what we would expect to see in 10 to 20 years’ time. The patient monitoring technology to deal with issues such as falls not only increases patient quality of care but safety. It is like looking at how health care will be provided in the future,” Dr. Wormald said.
Meanwhile, among the Methodist Otolaryngology faculty, Joshua Kain, M.D., is one of the high-end users of OPC 18 and agrees with visitors’ assessments. “I consider myself fortunate to do head and neck cancer surgery in an age where technology translates to meaningful improvements for those facing surgical treatments,” he said. Dr. Kain is an assistant professor of Otolaryngology, Weill Cornell Medical College and Houston Methodist Academic Institute. He specializes in Head and Neck Surgical Oncology and Microvascular Reconstructive Surgery.
One particular instance where technology is important, he said, is in throat cancer in young patients. Conventional approaches often would mean cutting bones or wide incisions just for access to a tight space. “The single-port robotic systems and microscopic equipment we have now eliminates that need in many cases. This can take a recovery that would be weeks and cut it down to days,” Dr. Kain adds.
Vice President of Operations Cathy Williamson said Houston Methodist is committed to creating an ideal operating room environment for the Department of Otolaryngology, Head and Neck Surgery that includes top-of-the-line technology in a comfortable most modern facility with unique personnel who have the skill needed for the OPC 18 ENT Service Line Team. “This is very special,” she said, “Even for the Texas Medical Center.”
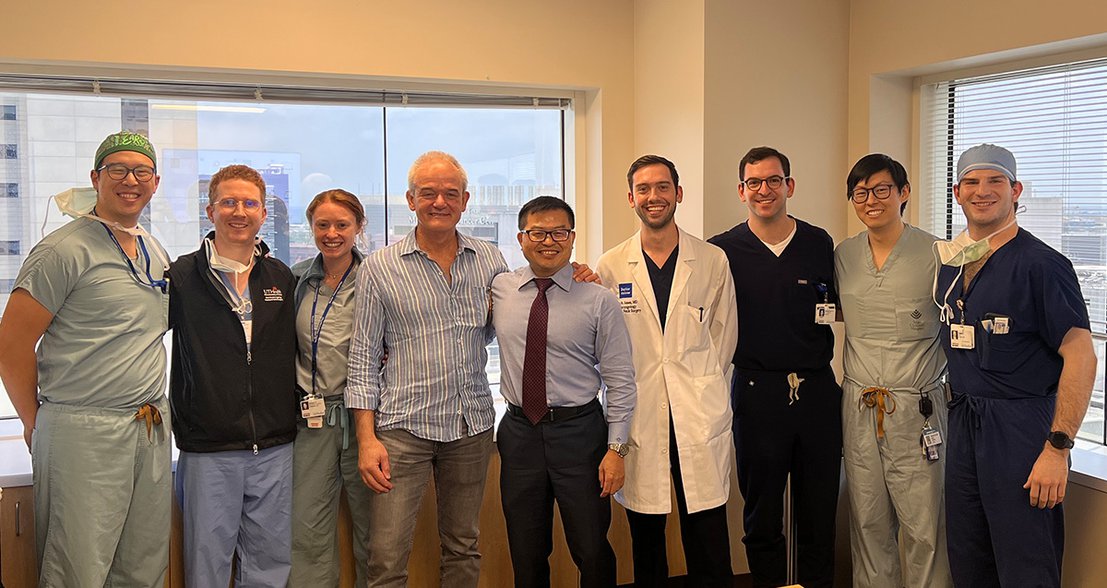
Drs. PJ Wormald and Mas Takashima in center.
The operating room was designed for maximum patient comfort and privacy with private preoperative rooms and recovery room space, large operating room suites, 4K monitors and camera technology for a range of cases, and best practice current equipment and supply support. This capability offers the Department faculty the best opportunity to handle safely and regularly all otolaryngology surgical cases required to benefit patients. It also covers ENT emergency services with lifesaving cases.
“The tour that I went on with Mas (Takashima) was a real eye opener,” Dr. Wormald said. “His vision is coming to pass and is extraordinary.”
According to Ms. Williamson, the surgical case volumes for ENT have increased beyond pre-COVID levels with significant growth continuing. “We’re building a good team; they are increasing their volume and are already asking for more OR space,” she added.
“This is one of the top priorities the hospital is focusing on and a big need for our community. It also ties in with our cancer program, which is one of our centers of excellence,” she said.
Otolaryngology, Head and Neck Surgery subspecialties include Facial Plastics, Neurotology, Head and Neck Surgery, Microvascular Surgery, Robotic Surgery, Laryngology, Rhinology, Sleep Surgery and related areas that require a highly skilled and trained surgical team. At Methodist, the Otolaryngology program has a dedicated staff of anesthesiologists, CRNAs, surgical techs, RNs and supply staff that exclusively works in the special service-line specific operating room and can handle anything from the most basic to the most complex and dangerous cases.
Travis Tingle, Director of the OPC 18 Perioperative Services, said the team has most of the technology on their wish lists especially with the DaVinci Single Port Robot that is making many small space surgeries more doable, successful and efficient.
“We have been outpacing ourselves every year. This has been our most active year ever,” Tingle said, pointing out that as the general population ages there is increased need for Otolaryngologic surgeries for hearing to maintain quality of life.
“We are very specialty driven,” Tingle said. “The ENT group has a powerful reputation; we meld very well together.”
Other equipment for our specialty include ORBEYE 4K 3D Orbital Camera System, the Video Rhinology and Endoscopic Sinus Surgery Suites, Leica Surgical Microscopes, complete lasers with CO2 and KTP and others for laryngology, special airway equipment and endoscopes.
The new camera system supports the immersive experience of the entire surgical team with space to work side by side and in the same orientation. The big screen 4K 3D visualization brings into focus anatomical details with four times the resolution of standard HD imaging. It gives the team the experience of true depth perception to reliably identify tissue boundaries, blood vessels and lesions with a variety of light modes such as blue light and infrared.
Technology here is what we would expect to see in 10 to 20 years’ time. The patient monitoring technology to deal with issues such as falls not only increases patient quality of care but safety. It is like looking at how health care will be provided in the future, Dr. Wormald said.
The camera system also brings ergonomic benefits for a more comfortable and natural working position including heads-up posture instead of necks bent for extended periods of time. The camera can be controlled via a foot switch and an agile autofocus and digital zoom always keeps the surgical field in focus, providing fast digital zoom in and out as needed.
The StealthStation ENT Navigation System offers electromagnetic technology for image-guided surgery from the most basic cases to the most complex. It provides 3D visualization of the patient’s anatomy and pathology with a simulated 3D endoscopic view of the sinuses to visualize anatomy, pathology and preoperative plans that are inaccessible with a traditional endoscope.
The Aura XP laser system allows controlled laser penetration for a wide range of soft tissue clinical applications for ears, nose and throat. Inner ear surgery can be performed precisely without disrupting tissue surround the Stapes bone while working in tight spaces. Nasal procedures are done with less bleeding and thermal damage than electrocautery. For the throat, it offers precise coagulation of diseased tissue while preserving soft mucosal layer of the vocal cords. Some uses include tonsillectomy, adenoidectomy, excision of laryngeal and pharyngeal tumors and lesions.
The UltraPulse CO2 laser is used to treat deep skin conditions like hypertrophic scars, deep skin resurfacing, scar revision and periorbital skin resurfacing.
“Many of the cancer surgeries and facial reconstructions we do routinely today were impossibilities as recent as 25 years ago without substantial harm and risk to a patient,” Dr. Kain said. “I get to take advantage of decades of advances and research that allow the same operations to be done safer, less-invasively, and with better outcomes than my own mentors had just years ago.
“We as modern surgeons are the direct beneficiaries of practicing in an era where these tools are at our direct fingertips both literally and figuratively,” he said.





