



clinical research
Not Alone: ‘Many patients assume they are the only ones struggling…’
Not Alone: ‘Many patients assume they are the only ones struggling…’
Educational pamphlets help pregnant women navigate their risk for pelvic floor disorders.
Educational pamphlets help pregnant women navigate their risk for pelvic floor disorders.
Pregnancy and childbirth are often referred to as life’s miracles. However, these miracles may come with a cost to pelvic floor health.
During pregnancy, childbirth and the postpartum period, many women develop pelvic floor disorders (PFDs). Yet, studies show that patients of child-bearing age don’t receive adequate information about these disorders, which can negatively impact health outcomes and quality of life.
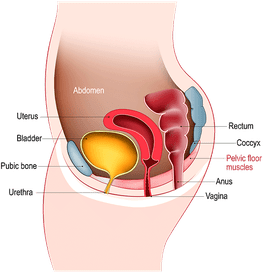
Pelvic floor disorders, which most commonly occur during pregnancy or childbirth, happen when the muscles or connective tissue of the pelvic area are weakened or injured.
That’s why Emily Rutledge, MD, Assistant Professor of Clinical Obstetrics and Gynecology at Houston Methodist, is working toward change.
“It can be challenging for obstetricians with such limited time during patient visits to adequately discuss PFDs with pregnant patients,” Rutledge explained. “Through our recent research study, we found that an intervention as simple as providing a pamphlet with tailored educational information can significantly increase pregnant patients’ PFD knowledge.”

Emily Rutledge, MD
In line with Houston Methodist’s I CARE Values, we want patients to know that we hear and see them as a whole person, even when the issues they are having are difficult to share. We respect our patients and are collectively dedicated to educating them about their current and future health risks, including PFDs.
Emily Rutledge, MD
Assistant Professor of
Clinical Obstetrics and Gynecology
The study, published in Urogynecology, involved randomizing 120 pregnant patients into two groups: one that only received written educational pamphlets, and one that received the same pamphlet and attended a virtual, interactive workshop led by a pelvic floor physical therapist.
Knowledge of PFDs were measured before and after the intervention using a validated questionnaire.
Participants in both groups increased their knowledge of PFDs, with no difference in knowledge between groups. These findings show that a simple intervention such as providing patients with well-written, tailored information does effectively increase their knowledge of PFD risk and treatment options.
“The hope is that these educational materials can foster a more streamlined conversation between healthcare providers and patients, so that patients can make better-informed decisions about their health,” Rutledge said.
Common Misconceptions
About PFDs
Facts about PFDs
Hover your mouse over each card below to discover common misconceptions about PFD.
While the study's findings are encouraging to obstetricians looking for an effective way to educate patients on PFDs, Rutledge was surprised by the study’s results.
“I think we underestimate how much we can teach patients with educational tools that are tailored to them,” Rutledge noted. “Many medical educational materials are geared towards patients who already have PFDs rather than informing women about their future risks. While unusual, our approach is necessary to help teach women about PFDs so that they can identify these issues if they occur in the future.”
Further research will focus on creating and testing PFD educational tools in various languages and education levels.
“Aligned with Houston Methodist’s I CARE Values, we want patients to know that we hear and see them as a whole person, even when the issues they are having are really difficult to share,” Rutledge said. “We respect our patients and are collectively dedicated to educating them about their current and future health risks, including PFDs.”
PFDs can impact patients’ everyday lives—whether its grappling with wearing sanitary pads, bringing a change of clothes or feeling embarrassed during sex. These potentially life-altering disruptions can even lead to patients shying away from friends and family and not discussing PFD symptoms with anyone, including healthcare providers. This social isolation, combined with minimal awareness of how common PFDs are among women, can contribute to patients assuming that they are alone in their struggles with PFD symptoms. All these factors make it supremely important for healthcare providers to actively ask patients about PFD symptoms to ensure they are addressed.
Rutledge E, Spiers A, Vardeman J, Griffin N, Nisar T, Muir T, Antosh DD. Educating Women About Pelvic Floor Disorders During Pregnancy From the First to the "Fourth Trimester": A Randomized Clinical Trial. Urogynecology (Phila). 2023 Sep 1;29(9):770-776. doi: 10.1097/SPV.0000000000001341. PMID: 37607311.
Share this story
Callie Rainosek, MS
January 2024
Related Articles
Clinical Research
Antibody to Fight Silent Killers
Joining forces to block MFAP5 protein in killer cancers






