


Precision Medicine
New theranostic shows promise for treating triple-negative breast cancer
The radiolabeled 64Cu/177Lu-DOTA-diZD small synthetic molecule revolutionizes treatment strategies for primary and metastatic tumors in aggressive triple-negative breast cancer by targeting angiogenic receptors.
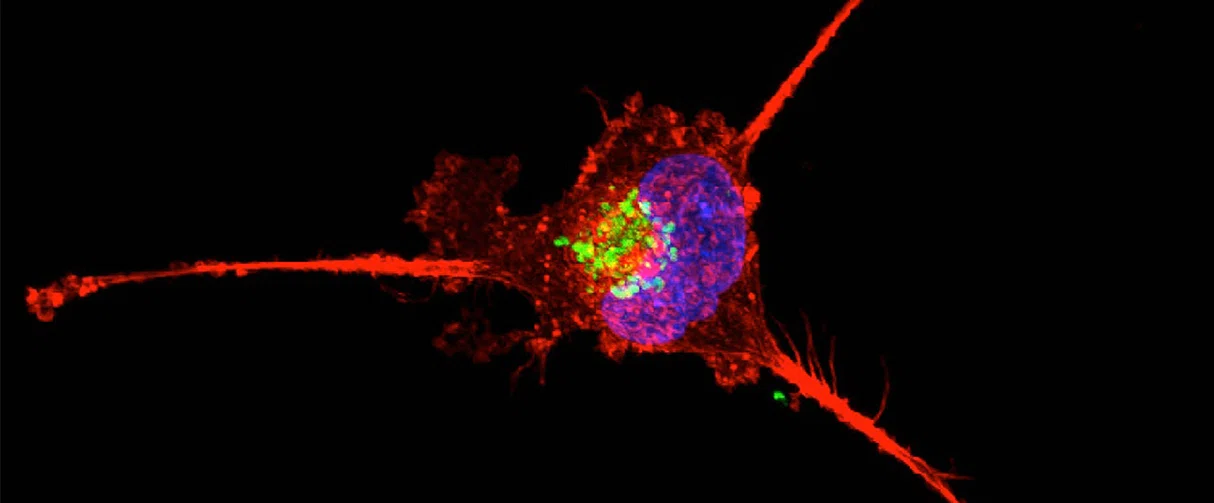
Triple negative breast cancer cell undergoing retraction and apoptosis
Triple-negative breast cancer (TNBC) is an extremely aggressive and metastatic sub-type of breast cancer seen commonly in young women of African descent and in breast cancer 1 gene mutation carriers that accounts for 10-20 percent of all breast cancer cases. The options for treating this form of cancer are limited, resulting in an exceedingly high mortality rate.
Most treatment options for breast cancer entail targeting three molecular targets - estrogen receptors, progesterone receptors, and human epidermal growth factor 2 receptors. TNBC cells do not have these markers, which hinders the development of tailored treatment options.
Angiogenesis — a crucial factor in cancer progression — is a promising therapeutic target for primary and metastatic TNBC. While a plethora of attempts has been made to control angiogenesis in solid tumors, they only have been modestly effective. Some success has been demonstrated with antibody-based targeted radionuclide therapies (TRT), although it has been limited by restricted infiltration into solid tumors, high-cost burden, and immunogenicity.
In a study recently published in the Journal of Medicinal Chemistry, Zheng Li, PhD, associate professor at the Houston Methodist Center of Bioenergetics, created a synthetic small molecule-based angiogenic TRT for TNBC treatment that improves upon the parental drug compound.

Zheng Li, PhD
The angiogenic-receptor-targeted TRT poses a promising therapeutic strategy in TNBC. Our work suggests that TNT has great potential to treat immunogenic cold TNBC, and further study is needed to optimize combination strategies with TNT, bearing in mind the elusive window for synergy and potential for added toxicity.”
Zheng Li, PhD, associate professor
Houston Methodist Center of Bioenergetics
Specifically, Li radiolabeled diZD, a vascular endothelial growth factor receptor (VEGFR) targeting agent with 177Lu for an angiogenesis-based TRT and 64Cu for positron emission tomography (PET) imaging in a preclinical TNBC murine model. Cell binding assays confirmed specificity and equivalent binding affinities of both 177Lu-DOTA-diZD and similarly constructed 64Cu-DOTA-diZD to cellular VEGFR2. Moreover, the binding of either of these was significantly enhanced relative to the parental drug compound ZD6474. This 64Cu/177Lu-DOTA-diZD theranostic pair demonstrated a notable antitumor efficacy, enhanced local tumor control, and greater survival rates in 4T1 tumor mouse models.
PET imaging revealed a surging diZD accumulation in the tumor of mice from 6 hours to 24 hours post-injection peaking at 48 hours. Further, diagnostic imaging of the 64Cu-DOTA-diZD revealed marked uptake in lung metastatic lesions as well as the lungs themselves suggesting a potential for both primary and metastatic tumor TRT using 177Lu-DOTA-diZD.
The volume of the tumors in 4T1 mice treated with 177Lu-DOTA-diZD were significantly reduced and survived significantly longer before reaching the study endpoint without systemic toxicity, relative to controls.
Antibody-based TRT for TNBC includes the immune checkpoint inhibitor against the programmed death receptor 1 (PD1). PD1 is expressed on the surface of tumor cells and is centrally involved in the tumor-induced suppression of the immune system.
To contrast the potency of the 64Cu/177Lu-DOTA-diZD TRT treatment with the anti-PD1 antibody immunotherapy, Li performed several comparative studies. First, expression of the proliferation biomarker Ki67 was markedly diminished in tumor tissues of 4T1 mice treated with 177Lu-DOTA-diZD, although it was present in the same treated with anti-PD1 immunotherapy. Second, CD4+ and CD8+ cell populations doubled post treatment with 177Lu-DOTA-diZD TRT whereas only a slim increase in these cell populations was observed post-treatment with anti-PD1 immunotherapy. This indicated that the anti-PD1 antibodies elicited a poor response in the 4T1 tumor-bearing mice. These results also shed light on a possible mechanism of action of the 177Lu-DOTA-diZD molecule – tumor microenvironment modulation and triggering of the adaptive immune response.
It is unclear if TRT and anti-PD1 immunotherapy can complement each other in terms of producing better treatment outcomes. It is speculated that radiation therapy inflects the tumor microenvironment and triggers the adaptive immune response, leading to infiltration of active immune cells and hence a better response to immunotherapy. However, studies of combinatorial therapies reveal disparate results. Studies on an immunoresponsive colon cancer model suggested improved survival and long-term tumor control with concurrent TRT/anti-PD1 immunotherapy as compared with sequential therapy. Further investigation on the potentials of TRT/anti-PD1 combinatorial immunotherapy with an emphasis on the optimization of the sequence or timing of administration is imperative.
TRT, such as the one developed by Li, extends several advantages. For instance, it causes less collateral damage as compared to external-beam radiotherapy and can also act on metastatic tumors not accessible with external radiation. The small molecule VEGFR-targeted TRT developed by Li can significantly enhance the treatment of immunogenic cold TNBC and possibly revolutionize the clinical management of metastatic TNBC.
Yuqian Huang, Zhen Yang, Feng Li, Hong Zhao, Chun Li, Nam Yu, Dale J Hamilton, Zheng Li. 64 Cu/ 177 Lu-DOTA-diZD, a Small-Molecule-Based Theranostic Pair for Triple-Negative Breast Cancer. J Med Chem. 2021 Mar 11;64(5):2705-2713. doi: 10.1021/acs.jmedchem.0c01957.
This work was supported by the Houston Methodist Research Institute (HMRI) and foundation. The authors thank the preclinical imaging core facility of HMRI. This research was funded in part through DoD BCRP Breakthrough Award (BC141561P1) (Z.L.) and Finger Distinguished Endowed Chair (D.H.).
Abanti Chattopadhyay, PhD, July 2021
Related Articles





