


outcomes research
Knee Surgery Goes Pro
Knee Surgery Goes Pro
1951 World Series. Game 2. Fifth inning.
In the outfield, Joe DiMaggio and Mickey Mantle are sprinting for a Willie Mays’ fly ball. Mantle stepped on an exposed drain and went down as DiMaggio made the catch.


One heart-stopping misstep left Mantle’s knee a mass of torn cartilage, ligaments and tendons, and he was carried off the field at the end of his first season in pro baseball.
The knees are well-suited for most of what we demand from them, but no one is harder on knee articular cartilage than a professional athlete. It’s no surprise then that the incidence of articular cartilage knee injuries is generally higher in athletes than nonathletes.
Injuries to articular cartilage are especially problematic for patients with high demands on their knees, causing pain and swelling that limit participation in high-level athletics. Articular cartilage is a thin, white, living tissue covering the ends of bones where they meet to form joints such as in the knee. It allows the bones to glide over one another without friction, protects the bones and enables smooth movement. Considering the inherent limits to healing within joints, managing damage to articular cartilage is particularly challenging. If severe, surgery is usually the only option.
Osteochondral allograft transplant—where an allograft osteochondral plug is fit in a congruent fashion to the patient’s articular surface—is an elegant surgical option to treat osteochondral lesions with a surface area of at least 2 cm2. This procedure provides a viable choice for injuries with extensive subchondral edema, even with prior marrow stimulation and it carries less risk of donor site morbidity. Current literature offers reassuring outcomes of osteochondral allograft transplant in general athletes, but little data exist on the outcomes in high-level, professional athletes.

By focusing on a unique patient population with the highest demands on their knees, this study more conclusively shows that osteochondral allograft transplant in professional athletes can result in a high rate of return to play at a similar or higher level as pre-surgery, even when performed with concomitant procedures such as meniscal allograft transplant.

Sachin Allahabadi, MD
Assistant Research Professor
of Clinical Orthopedic Surgery
Understanding the success or failure of osteochondral allograft transplants in professional athletes is critical for performance expectations and career longevity. However, present literature relies on studies with enough independent variables (beyond the treatment itself) influencing an athlete’s return to preinjury status; however, caution must be used in interpreting the results. To investigate osteochondral allograft outcomes in professional athletes without as many confounding factors, Sachin Allahabadi, MD, Assistant Professor of Clinical Orthopedic Surgery, worked with a team at Rush University Medical Center in Chicago on a study evaluating the experience of his mentor and senior surgeon, Brian J. Cole, MD, MBA, in treating professional athletes with osteochondral allograft transplant, including analyzing clinical outcomes and return to sport.
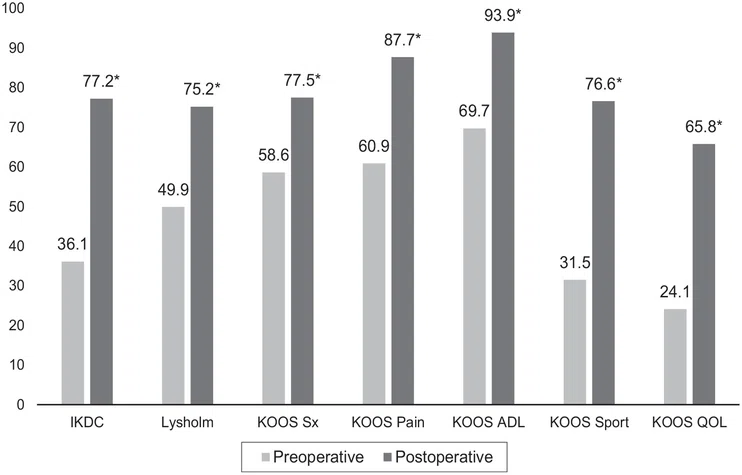
Patients demonstrated statistically significant postoperative improvements at the most recent time point for all PROs (P < .01) Mean patient-reported outcome measure scores after primary osteochondral allograft transplant of the knee in professional athletes. *Significant improvement from preoperative to postoperative (P < .01). ADL, activities of daily living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; QOL, quality of life; Sport, sport and recreation; Sx, symptoms. From paper
With Allahabadi as first author, the study included a retrospective review of professional athletes who underwent primary osteochondral allograft to the knee between January 1, 2001, and January 1, 2021, by a single surgeon. All procedures were performed by the senior author (Cole), a fellowship-trained orthopedic surgeon with a high-volume referral-based practice in cartilage restoration. To be included in the study, athletes had to play at the professional level and have a minimum of two years of follow-up. Fifteen professional athletes representing a variety of sports participated. The majority had undergone prior surgeries to the operative knee.
Patients demonstrated statistically significant postoperative improvements at the most recent time point for all PROs (P < .01). Eleven returned to sport at a mean of 1.22 years, and of the eight undergoing isolated osteochondral allograft, seven returned at 1.28 years. Ten athletes returned to sport at the same level or higher as before surgery. Significant improvements were observed in all assessed patient-reported outcome scores. Two of the three patients who underwent concomitant meniscal allograft transplant were able to return to sport at the same level or higher than pre-surgery. Three underwent second-look arthroscopy, one of whom underwent cartilage debridement of the osteochondral allograft.
High-level athletes can expect significant postoperative improvement in clinical outcomes with this procedure.
“By focusing on a unique patient population with the highest demands on their knees, this study more conclusively shows that osteochondral allograft transplant in professional athletes can result in a high rate of return to play at a similar or higher level as pre-surgery, even when performed with concomitant procedures such as meniscal allograft transplant,” said Allahabadi.
Sachin Allahabadi, MD, Ryan Quigley, MD, Landon Frazier, MD, Kaitlyn Joyce, and Brian J. Cole, MD, MBA
Heather Lander, PhD
December 2024
Related Articles








