


PRECISION MEDICINE
Jumpstarting dysfunctional regulatory T cells into action could help treat Parkinson’s disease
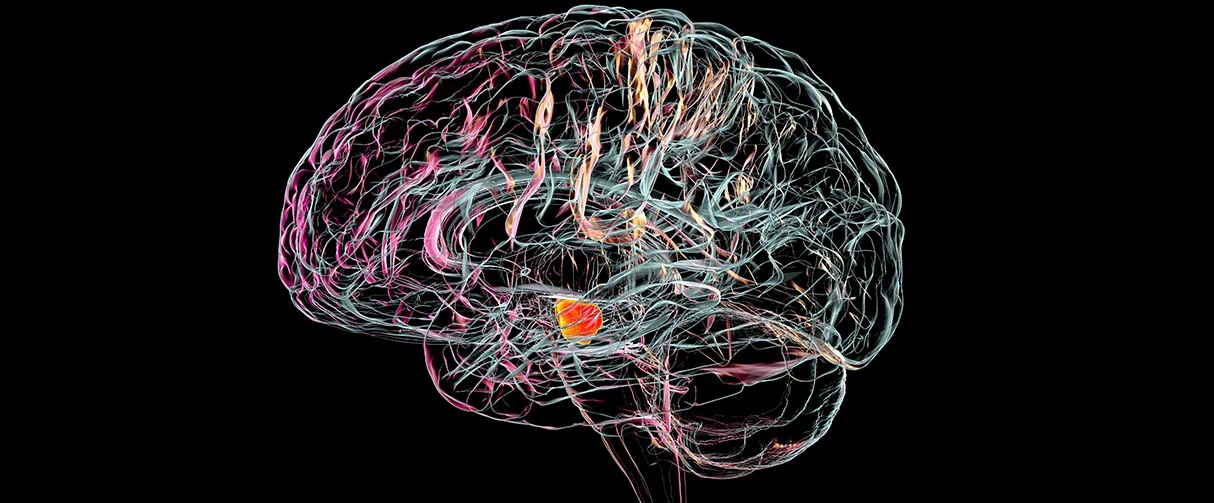
First described as shaking palsy in 1817 by the English surgeon James Parkinson, his namesake disease is infamous for its debilitating motor symptoms stemming from the untimely death of the midbrain’s dopaminergic neurons. A major player linked to this progressive neuronal damage is chronic inflammation that is perpetuated by an altered, pathological immune response within the Parkinson’s brain.
In a study published in npj Parkinson’s Disease, Houston Methodist researchers provide evidence that the regulatory T immune cells, or Tregs, are not just reduced but also dysfunctional in Parkinson’s disease. Consequently, these otherwise immunosuppressive cells are unable to dial down the inflammation in the central nervous system.
However, they also showed that peripheral Tregs can be successfully activated and expanded ex vivo. These restored Tregs, they said, can then be potentially used to suppress pro-inflammatory immune cells.
“We have shown proof of concept that we can take the dysfunctional Tregs and then activate them to make them hyper suppressive, providing a potential therapeutic route to treating Parkinson's disease,” said Aaron Thome, PhD, assistant research professor of neurology. “From here, our next step would be to inject these cells back into the patient and investigate not only if it is safe and well-tolerated, but also if infusion of functional Tregs can halt the progression of the disease.”
Like elsewhere in the body, inflammation within the brain is typically a part of immune responses needed for tissue maintenance and repair. However, if the inflammation is prolonged due to neurodegenerative diseases or traumatic brain injuries, then progressive neuronal damage occurs. Further, chronic inflammatory changes can increase the permeability of the blood-brain barrier to peripheral immune cells, amplifying the ongoing neuroinflammation.
In Parkinson’s disease, dopamine-producing neurons in the substantia nigra pars compacta are the most vulnerable to damage from inflammation. The initial immune response is speculated to be triggered by the death of dopaminergic neurons due to an accumulation of misfolded alpha-synuclein proteins in their cell bodies.
To clear up the dead tissue and debris, microglia, the resident innate immune cells of the brain, sweep into action. But with time, increasing aggregations of toxic conformations of alpha-synuclein cause more cell death, recruiting even more immune cells and eventually setting off chronic inflammation. Furthermore, misfolded alpha-synuclein can even directly activate pro-inflammatory immune cells to drum up neuroinflammation.
The ability to successfully expand Tregs outside the body and restore their suppressive function allows us to consider infusing the functionally suppressive Tregs in Parkinson’s disease.”
Aaron Thome, PhD
Assistant Research Professor of Neurology
Houston Methodist
The body produces specialized T lymphocytes to suppress pro-inflammatory immune responses and restore homeostasis. In neurodegenerative diseases, like Alzheimer’s disease and amyotrophic lateral sclerosis (ALS), however, these regulatory cells are dysfunctional and fail to suppress the marked inflammation.
“Even in Parkinson’s disease, there is some history indicating that Tregs are altered but nothing definitive,” said Thome. “And so, we decided to do a larger study to investigate Treg dysfunction in patients with this neurodegenerative disease.”
For their study, the researchers compared T cell populations in the peripheral blood that was derived from 39 patients with Parkinson’s disease with those from 31 age-matched, healthy controls. They found that compared to controls, patients with Parkinson’s had a significant decline in the number of Tregs with disease progression. Furthermore, these cells had reduced expressions of CD25 and FOXP3 proteins that are essential proteins for Treg health and function.
Concomitantly, gene expressions of pro-inflammatory cytokines, such as interferonγ, tumor necrosis factor, and interleukin-2 (IL-2), were elevated in effector T cell population along with direct evidence of Treg dysfunction when co-cultured with inflammatory cells in vitro, thus, implicating that Tregs were impaired and unable to sufficiently suppress pro-inflammatory immune cells in these patients.
To investigate if the dysfunctional Tregs can be reactivated, the researchers isolated and cultured the patient Tregs using IL-2, CD3/CD28 activation beads, and rapamycin to activate and expand the Tregs ex vivo. Next, the team co-cultured these expanded Tregs with proliferating T effector cells and proinflammatory myeloid cells. They found that the suppression of the Tregs markedly increased after expansion, resulting in enhanced suppression of T effector cell proliferation and suppression of pro-inflammatory myeloid cells via reduction in gene expression of a variety of proinflammatory cytokines, including that of IL6 by 89%.
The researchers noted that the next step in their research would be a phase 1 clinical study in which the dysfunctional Tregs are taken out from peripheral blood from Parkinson’s patients, expanded as per the protocols delineated in their study and then returned to the patient.
“The ability to successfully expand Tregs outside the body and restore their suppressive function allows us to consider infusing the functionally suppressive Tregs in Parkinson’s disease,” said Thome. “This approach is already being tested with promising results in Amyotrophic Lateral Sclerosis at Houston Methodist and, in principle, we can do the same for our Parkinson’s patients.”
The researchers noted that the Treg cell-based therapy for Parkinson’s disease has precedent. This procedure has been previously shown to be safe and tolerable in clinical trials for ALS jointly conducted at Houston Methodist and Massachusetts General Hospital Neurological Clinical Research Institute.
Aaron Thome, Farah Atassi, Jinghong Wang, Alireza Faridar, Weihua Zhao, David Beers, Eugene Lai, Stanley Appel. Ex vivo expansion of dysfunctional regulatory T lymphocytes restores suppressive function in Parkinson's disease. NPJ Parkinsons Disease (2021) 7(1):41. doi: 10.1038/s41531-021-00188-5.
This study was partly funded through philanthropic contributions from the Parkinson’s Cell Therapy Research Fund.
Vandana Suresh, PhD, March 2022
Related Articles








