It Takes a Village
It Takes a Village
MITIESM’s Maternal and Infant Simulation Instructor Course gives providers a chance to get ahead of childbirth-related mortality and morbidity.
MITIESM’s Maternal and Infant Simulation Instructor Course gives providers a chance to get ahead of childbirth-related mortality and morbidity.
Innovative Education


Maternal mortality and morbidity are on
the rise in the US, and Texas ranks among
states with the highest rates.
According to the Texas Medical Association, the leading cause of maternal death and illness in Texas is lack of access to health care. A recent report found Texas to be last among the 50 states in percentage of women of childbearing age with health insurance (73.6%) and primary care provider (57%).
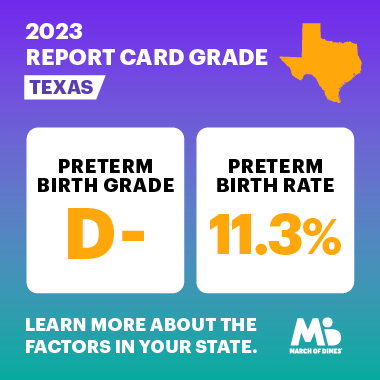
Health care disparities among pregnant women in Texas are also striking. In 2013, when Texas first began tracking deaths and severe illness or injury from pregnancy and childbirth, Black women were twice as likely as white women, and four times as likely as Hispanic women, to die from pregnancy-related causes. Despite increased research, awareness and political attention, a decade later these disparities remain. In 2023, the March of Dimes report card gave Texas a grade of D- for maternal and infant health.
The March of Dimes report card highlights key indicators to describe the current state of maternal and infant health. In 2023, maternal mortality, leading causes of infant death and data describing selected risk factors for preterm birth were included for the first time among the metrics.
The need for improving maternal-fetal outcomes is clear, and Houston Methodist has been, and remains, committed to the cause. The most recent Houston Methodist initiative focused on improving childbirth outcomes is MITIESM’s Maternal and Infant Simulation Instructor Course for health care providers.
Simulation-based medical training can lead to a reduction in errors, increased safety, improved judgment in the clinic and increased self-confidence. By immersing learners in a realistic environment, simulations give providers the opportunity to utilize cognitive, behavioral and technical skills needed in clinical practice. It also gives learners a safe place to experience high-risk, low frequency scenarios and analyze and troubleshoot issues that arise.
The Maternal and Infant Simulation Instructor Course is designed to train functional teams from within campuses systemwide on simulation-based scenarios to treat mother and baby during life-threatening events. As an instructor course, the focus is on training system leaders in simulation scenario design and post-encounter debriefing. In addition, trainees will experience high reliability simulations designed to standardize care around evidence-based best practices for maternal hemorrhage, HTN/ eclampsia, and neonatal resuscitation.
Randolph H. Steadman, MD
Made possible by Houston Methodist Research Institute funding to improve quality of patient care, and led by Randolph H. Steadman, MD, MS, Carole Walter Looke Centennial Chair in Anesthesia and Critical Care, this MITIE course itself is a metaphor for how critical teamwork is to patient outcomes, especially in maternal-fetal medicine. Before the simulations can take place, a team must design the scenario being simulated, and coordinate with the audio-visual and technical teams to ensure the simulation takes place as designed. It’s no small feat. The mannequins are programmable and can move and respond to medical interventions. However, each simulation requires precision in scenario design and programming.
The course debrief post-simulation is just as critical. Trainees and instructors meet to review and discuss how the simulation went.
“It’s an opportunity to discuss what went well and what went wrong with the delivery of the scenario as well as with the medical treatment administered,” said Cristina Martin, MSN, RN, Director of the Childbirth Center at Houston Methodist Hospital Sugar Land, “It benefits trainees and instructors.”
Simulation and case-based learning represent an important means of preparing maternal-fetal medicine providers to manage life-threatening severe morbidity scenarios.
“It gives providers practice working in teams under emergency scenarios so that if it happens for real, the team can work together more effectively to improve patient outcomes,” said Steadman. Obstetric simulation training leads to improved interdisciplinary teamwork and patient outcomes with fewer medical and communication errors.
Heather Lander, PhD
February 2024
Related Articles