


Restorative medicine
Lessening Pain After Knee Replacement Surgery
Infusing morphine and vancomycin directly into the tibia during knee replacement reduces pain and pain medication needed after surgery.

In a study, Houston Methodist researchers present clinical evidence supporting the safety and efficacy of injecting pain medication directly into the tibia during knee replacement surgery for better postoperative pain management.
The double-blind, randomized trial detailed in The Journal of Arthroplasty revealed that patients receiving a mixture of morphine and the antibiotic vancomycin into the tibia of their knee joint have lesser pain post-surgery compared to those that did not receive the intraosseous infusion.
“Despite many technological advances, controlling pain after total knee arthroplasty can be challenging; most patients experience considerable pain and discomfort, especially in the first couple of weeks into their recovery,” Kwan “Kevin” Park, MD, orthopedic surgeon at Houston Methodist. “Intraosseous infusion allows us to control pain pre-emptively so that patients don't have to take as much pain medicine later on.”
Total knee replacement is the recommended treatment to alleviate chronic pain caused by damage to the knee joint from arthritis or injury. According to the 2021 American Joint Replacement Registry Annual Report, primary knee replacement surgeries accounted for 54.5% of the nearly 2 million hip and knee replacement procedures performed between 2012 and 2020.

Kwan "Kevin" Park, MD
Orthopedic Surgeon at Houston Methodist

Francesca Taraballi, PhD
Assistant Professor of Orthopedic Surgery and Director of Houston Methodist’s Center for Musculoskeletal Regeneration
Despite the high frequency and favorable outcomes of the surgical procedure, the manipulation of soft tissue and resurfacing damaged bones during knee replacement causes pain in the early postoperative periods.
“Twenty years ago, patients would remain in the hospital for several days after their surgery and receive extremely high-dose narcotics to help with their postoperative pain,” said Park. “But there has been a paradigm shift; patients are often discharged the same day after knee replacement surgery, and we use multimodal pain management techniques that work much better for pain control and require fewer narcotics.”
These multimodal regimens, he added, often include a combination of medications, such as nonsteroidal anti-inflammatory drugs, opioids and neurogenic agents, administered both pre-emptively and after the surgery. However, opioid medications, although very effective in managing pain, have known side effects, like constipation and nausea with some people even allergic to opiates. Furthermore, a consensus on the optimal preoperative protocol to mitigate pain is lacking.
Previously, the researchers demonstrated that injecting vancomycin directly into the tibia before surgery helped in reducing infection by reaching a higher concentration of the drug in the knee. Motivated by this success, they investigated whether delivering both morphine and vancomycin into the tibial bone could improve postoperative pain management.
For the study, the team included 48 patients needing total knee replacement surgery. Of these patients, half were randomly assigned to receive vancomycin and morphine intraosseously using an infusion device that was inserted into the tibial tubercle region. The remaining were only administered vancomycin. Post-surgery, the researchers monitored patient-reported pain, nausea and opioid use for up to 14 days after surgery. Also, Park’s team collaborated with Francesca Taraballi, PhD, assistant professor of orthopedic surgery and director of Houston Methodist’s Center for Musculoskeletal Regeneration to measure the serum levels of morphine and the inflammatory marker interleukin-6 in all study participants for 10 hours after the operation.
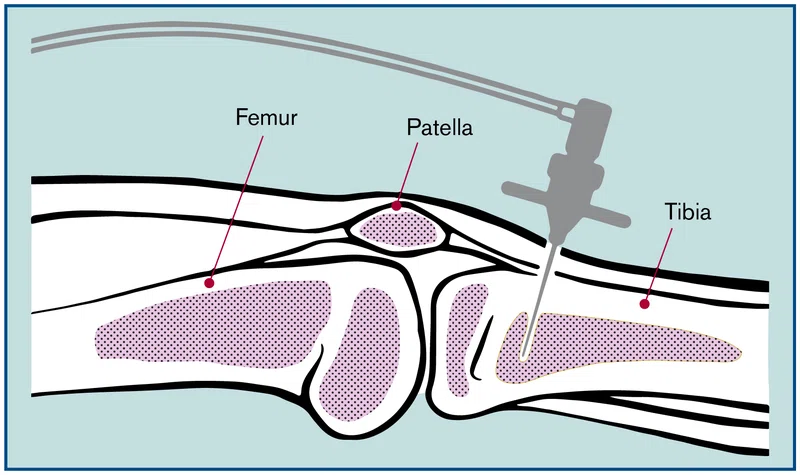
A power driver is used to inject a combination of vancomycin and morphine into the tibia during knee replacement surgery.
Upon analyzing their data, the researchers found that the patients who were given morphine in the tibial bone had lower pain scores after their knee replacements compared to those that did not. Further, these patients also reported having less pain for several days and had similar serum interleukin-6 levels as the control group. Taken together, although the patients that received pain medication intraosseously had a comparable inflammation, these patients were taking less pain medication post-surgery.
Park noted that the intraosseous infusion of opiates could potentially even facilitate a swift recovery of the knee joint.
“By infusing pain medication intraosseously we're able to reduce postoperative pain for up to two weeks, the number of pain pills patients need and even possibly improve the function of the knee over time,” he said. “Our technique can also improve the multimodal pain management protocol we have been using for knee replacement over the years.”
Brozovich AA, Incavo SJ, Lambert BS, Sullivan TC, Wininger AE, Clyburn TA, Taraballi F, Park KJ. Intraosseous Morphine Decreases Postoperative Pain and Pain Medication Use in Total Knee Arthroplasty: A Double-Blind, Randomized Controlled Trial. J Arthroplasty. 2022 Jun;37(6S):S139-S146. doi: 10.1016/j.arth.2021.10.009. Epub 2022 Mar 7. PMID: 35272897.
Vandana Suresh, PhD, June 2022
Related Articles
RESTORATIVE MEDICINE
Novel Vascular Engineering Platforms Are a Boon for Bioengineering
Owing to a dearth of donated organs for transplantation, scientists at Houston Methodist have made a significant breakthrough the field of organ engineering

RESTORATIVE MEDICINE
Improved Translational Models to Probe Brain Hemorrhage
A battery of validated rodent behavioral tests now facilitates investigating the underpinnings of neurocognitive deficits after a subarachnoid hemorrhage.






