


Outcomes Research
Gut Microbiota as a Therapeutic Target
Gut Microbiota as a Therapeutic Target
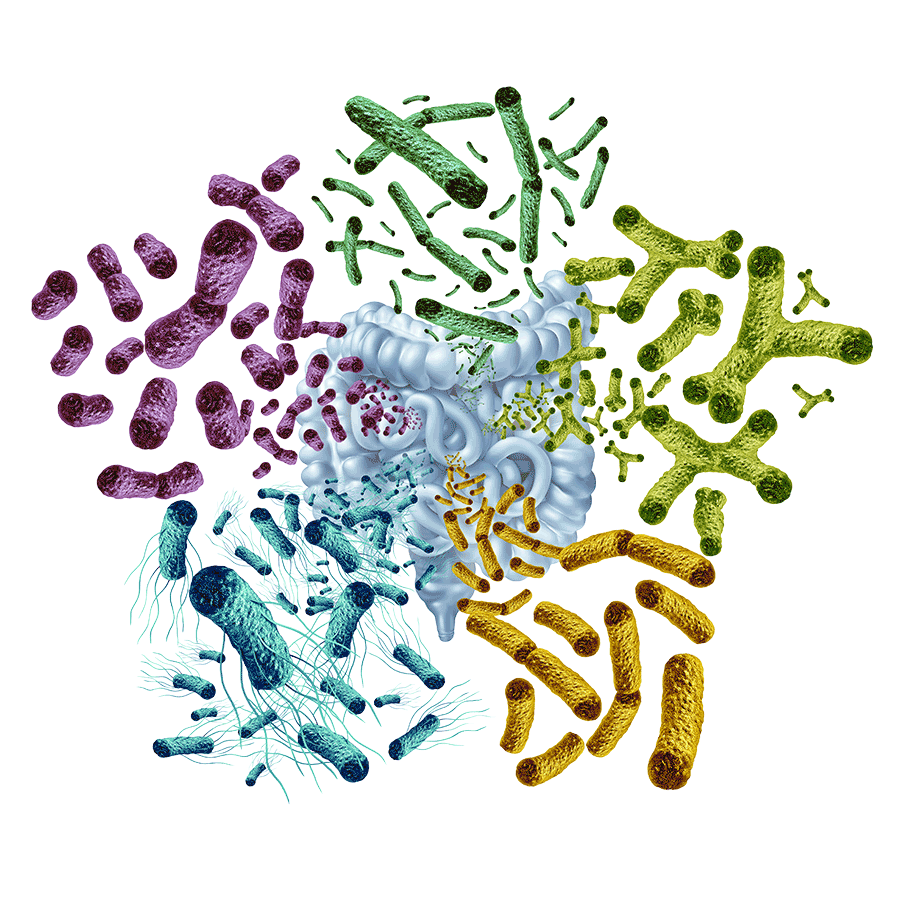
Gut microbiota refers to the trillions of microorganisms that reside in the human digestive tract in a dynamic balance. The composition and function of the gut microbiota are critically important, as an imbalance (gut dysbiosis) can lead to myriad diseases, including inflammatory bowel disease, irritable bowel syndrome, autoimmune disorders, type 2 diabetes, cardiovascular diseases, neurological diseases and certain cancers.
Neurodegenerative diseases are also linked to gut dysbiosis because of the bidirectional, homeostatic communication between the central nervous system and the gut microbiome.
Sonia Villapol, PhD
Sonia Villapol, PhD, Assistant Professor of Neurosurgery, is focused on modulating gut microbiome dysbiosis to reduce neurodegeneration. Using microbiome sequencing data, she builds precision-based clinical diagnostic and prediction models. Additionally, Villapol and her team are investigating peripheral mechanisms that link brain injury to long-term degeneration, neuroinflammation induced by traumatic brain injury (TBI), and using nanoparticles as a theranostic tool to target brain inflammation. By understanding the inflammatory and neurodegenerative mechanisms, Villapol aims to develop therapeutic solutions to restore normal brain function. Specifically, efforts are underway to find innovative treatments for Alzheimer’s disease (AD).
The gut microbiome plays a significant role in myriad biological processes, including health maintenance, digestion, immune system development, diseases, brain function, metabolism and aging. The intricate network of interactions between the gut, gut microbiome and the central nervous system (CNS) is called the microbiota gut-brain axis. The microbiota-gut-brain axis regulates glial functions and therefore is a phenomenal target to manipulate the progression of neurodegenerative diseases.
The Villapol laboratory’s efforts are heavily focused on TBI. Any brain injury caused by an external force , such as falls, car accidents, gunshot wounds or contact sports, are referred to as TBIs. According to the Centers for Disease Control and Prevention, there are about 190 TBI-related deaths daily on average in the United States. Using a preclinical TBI model, Villapol concluded that TBI can cause disturbances in the gut microbiota and lipid metabolism in the liver.
Villapol believes that the brain can be protected from the adverse effects of TBI by modifying the composition of the gut microbiome.
“By understanding and intervening in the gut-brain-liver axis, researchers and medical practitioners could develop strategies to improve outcomes for individuals affected by TBI,” commented Villapol.
Here are a couple of additional conclusions:
- Probiotic therapy can mitigate neuroinflammation and improve motor, anxiety and depression-like behavior post-TBI.
- Probiotic treatment induces gender-dependent neuroprotection post-TBI.
According to Villapol, “Our results underscore the potential of probiotic interventions as a viable therapeutic strategy to address TBI-induced impairments, emphasizing the need for gender-specific treatment approaches.”
Gut dysbiosis is strongly correlated with neuroinflammatory diseases. Specific neuroinflammatory diseases associated with the gut microbiome include multiple sclerosis, AD, and Parkinson’s disease.
A hallmark of several neurological diseases is impairment of the blood-brain barrier that is critical for brain homeostasis. This causes harmful proteins such as beta amyloid plaques and tau tangles to accumulate in the brain while also preventing effective treatment using the blood stream. Under these circumstances, nanomedicine becomes a promising approach. Villapol developed a novel delivery system that uses biomimetic nanoparticles for drug delivery as well as diagnostics for AD and brain injury.
According to Villapol, “Biomimetic nanoparticles are a promising tool that can accelerate a therapy's translation more efficiently than cellular or exosome‐based techniques due to the ease of fabrication, purification, and similarity between the different nanoparticle batches. Relevant differences in nanoparticle biodistribution after brain trauma in filtering organs suggest a potential local and systemic future targeting strategy. Biomimetic nanoparticles could be strong candidates for acute pharmacologic treatment in TBI patients.”
“By observing the infiltration of nanoparticles into inflamed tissues, we can design how to overcome the therapeutic challenges of TBI using pharmacological therapy targeting specific inflammatory mechanisms,” Villapol added.
Active areas of research in the Villapol lab include:
- Microbiota-targeted approaches to resolve dysbiosis-induced AD neuropathology following brain injury
- Investigating peripheral inflammation on brain damage in a sex-dependent manner
- Gut microbiota diagnostics for concussions in athletes who play contact sports
- Exploring the functionality of biomimetic nanoparticles as a theranostic tool for brain injury and AD
- Intranasal delivery of telomerase reverse transcriptase mRNA for TBI therapy
- Precision-based microbiota therapy for brain injuries and AD
- Spaceflight effects on the gut-brain axis and immune functions
- Exploring microbial signatures for neurological manifestations in long COVID Patients.
- CRISPR-lipid nanoparticles-based treatment for TBI
- Exploring novel synergies between gut microbiome alterations after deep brain stimulation and cellular transplantation as a potential treatment of Parkinson’s disease and TBI
Additionally, Villapol and her team performed gut microbiome profiling on samples from 124 hospitalized COVID-19 patients using full-length 16S rRNA gene sequencing and found significant associations between mental health status, systemic inflammation and gut dysbiosis.
“The relationship between the gut-brain axis, gut microbiota, and psychiatric disorders, such as depression and anxiety, remains an area of active research and debate within the psychiatric community. While recent studies suggest that gut microbiota alterations may influence brain function and contribute to depressive and anxiety symptoms, the underlying mechanisms are not yet fully understood. Randomized controlled trials are necessary to assess the effectiveness of microbiome-targeted therapies, such as probiotics and dietary interventions,” Villapol commented.
For further information on TBIs and Dr. Villapol’s work on this topic, please see the following papers:
Vonder HC, Celorrio M, Martens KM, Friess SH, Villapol S, Urban R, Pyles R, Mychasiuk R, Simon D, Dave A. The gut microbiome as a modulator of traumatic brain injury pathology and symptoms. J Neurosci. 2025;0(0):e1337252025.
Holcomb M, Marshall A, Flinn H, Lozano M, Soriano S, Gomez-Pinilla F, Villapol S. Probiotic treatment causes sex-specific neuroprotection after traumatic brain injury in mice. J Neuroinflammation. 2025;22(1):114.
Scalzo PL, Marshall A, Soriano S, Curry K, Dulay M, Hodics T, Quingly EMM, Treangen TJ, Villapol S. Gut microbiome dysbiosis and immune activation correlate with somatic and neuropsychiatric symptoms in COVID-19 patients. J Transl Med. 2025;23(1):327.
Lopez-Espinosa J, Park P, Holcomb M, Godin B, Villapol S. Nanotechnology-driven therapies for neurodegenerative diseases: a comprehensive review. Ther Deliv. 2024;15(12):997-1024.
Abanti Chattopadhyay, PhD
November 2025
Related Articles





