


Clinical Research
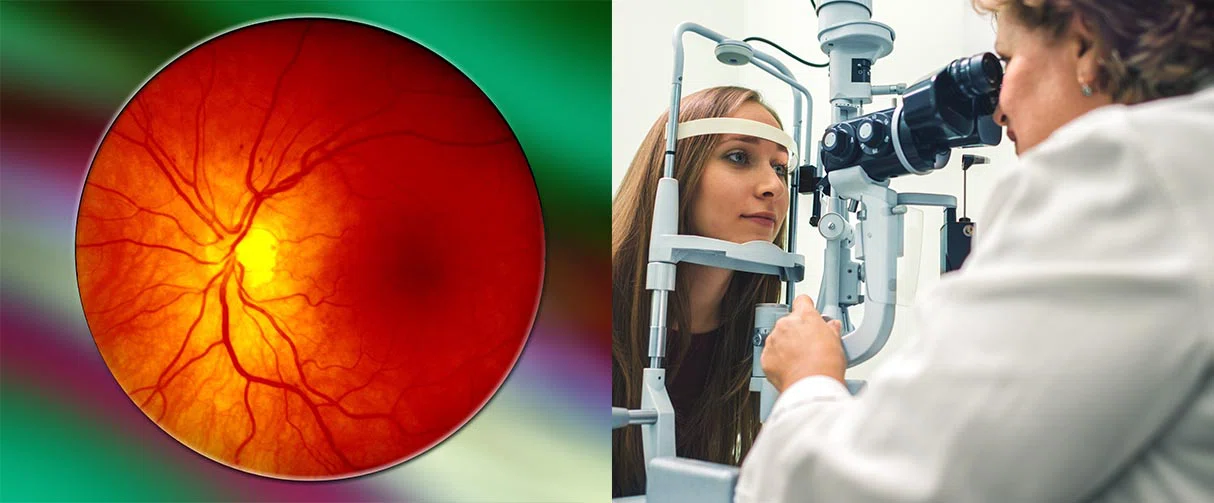
Improved Options for Patients with Severe Retinal Vascular Disease
In Phase III clinical trials, Faricimab met noninferiority endpoints over a current drug, aflibercept, to treat diabetic macular edema and neovascular age-related macular degeneration.
A new drug, faricimab, recently received FDA approval for the treatment of diabetic macular edema and neovascular age-related macular degeneration following the publication of primary results in four major phase III clinical trials, as reported in The Lancet.
The researchers demonstrated that faricimab met noninferiority endpoints over a current drug, aflibercept, while demonstrating robust vision gains, anatomical improvements and potentially longer intervals between dosing.
“It’s quite unusual to obtain simultaneous FDA approval for two common diseases, and I think it speaks to how well suited this particular drug is for the job of treating exudative retinal diseases,” said Charles Wykoff, MD, PhD, a Houston Methodist ophthalmologist and the principal investigator of the two nearly identical diabetic macular edema trials, YOSEMITE and RHINE.

Charles Wykoff MD, PhD
Associate Professor of Clinical Ophthalmology,
Houston Methodist
Diabetic macular edema and neovascular age-related macular degeneration are the leading causes of irreversible blindness in the U.S., with 4 million adults actively affected and 10 million more at risk of severe retinal vascular disease. Both diseases are characterized by abnormal blood vessels that leak in the retina, causing a buildup of fluids and consequently a progressive loss of vision.
The most common treatment to arrest blood seepage is anti-vascular endothelial growth factor A (anti-VEGF-A) medications that are delivered into the eye by intravitreal injection. These drugs have been a remarkable breakthrough, said Wykoff, changing the epidemiology of blindness and the prognosis of patients with diabetic macular edema and neovascular age-related macular degeneration.
Despite the effectiveness of anti-VEGF-A medications, certain drawbacks made treatment adherence and widespread adoption a significant challenge.
“Patients require an injection typically every four to 12 weeks, often indefinitely,” said Wykoff. “That is a substantial burden for patients, caregivers and eye care providers alike and a limitation of current therapeutics that has prevented us from fully realizing the potential of these drugs in the real world. Many of these patients face significant comorbidities and mobility issues related to advanced age or conditions associated with diabetes.”
Unlike anti-VEGF-A medications that target a single biochemical signaling pathway, faricimab, an angiopoietin-2 and VEGF-A bispecific antibody, blocks two key signaling pathways that are implicated in the pathogenesis of diabetic macular edema and neovascular age-related macular degeneration. In particular, by inhibiting angiopoietin-2, native angiopoietin-1 can bind to the endothelial receptor tyrosine kinase transmembrane receptor Tie2, leading to increased intracellular signaling that improves vascular leakage and drives stabilization of the blood-retinal barrier, reductions in inflammation and improved cell survival.
In preclinical studies and three Phase II clinical trials concluded in 2019, the dual pathway inhibition demonstrated the potential for increased vascular stability and greater reductions in vascular leakage, neovascularization and inflammation over VEGF-A inhibition alone.
“We wanted to test the durability of this novel drug using methods common in clinical practice, where you treat consistently until you achieve optimal outcomes, then titrate the frequency to meet individual patient needs,” explained Wykoff.
The diabetic macular edema trials were the first to incorporate a flexible, individualized treatment interval approach in a double-masked manner. Nearly 1,900 patients across 353 sites worldwide were randomly assigned to receive either (a) faricimab every eight weeks, (b) aflibercept (a VEGF-A antagonist) every eight weeks or (c) faricimab per personalized treatment intervals.
By the end of the one-year study period, more than 50% of patients in the personalized treatment interval groups could go up to 16 weeks between treatments without losing vision gains, and 70% could go up to 12 weeks or longer.
Faricimab, the researchers found, produced a more sustained effect than anti-VEGF-A monotherapies, like aflibercept, with faricimab demonstrating efficacy at up to 16-week intervals. In the future, additional studies are planned to examine the potential to extend treatment intervals even further in some patients.
Parallelly, in neovascular age-related macular degeneration phase III clinical trials, TENAYA and LUCERNE, led by Jeffrey Heier from Ophthalmic Consultants of Boston, 80% of patients receiving faricimab maintained their best-corrected visual acuity at 12-week or longer intervals with 45% maintaining it at 16-week intervals.
In January, Vabysmo (faricimab-svoa) became the only injectable eye medicine approved simultaneously in the U.S. for diabetic macular edema and neovascular age-related macular degeneration, with flexible dosing regimens based on patient need. Vabysmo is manufactured by Genentech, a subsidiary of F. Hoffmann-La Roche, who provided funding for the studies.
Wykoff CC, Abreu F, Adamis AP, Basu K, Eichenbaum DA, Haskova Z, Lin H, Loewenstein A, Mohan S, Pearce IA, Sakamoto T, Schlottmann PG, Silverman D, Sun JK, Wells JA, Willis JR, Tadayoni R; YOSEMITE and RHINE Investigators. Efficacy, durability, and safety of intravitreal faricimab with extended dosing up to every 16 weeks in patients with diabetic macular oedema (YOSEMITE and RHINE): two randomised, double-masked, phase 3 trials. Lancet. 2022 Feb 19;399(10326):741-755. doi: 10.1016/S0140-6736(22)00018-6. Epub 2022 Jan 24. PMID: 35085503.
Eden McCleskey, June 2022






