Outcomes research
Connecting the links between flu and heart disease
Houston Methodist researchers discuss impact of low influenza vaccine rates on patients with cardiovascular disease
Houston Methodist researchers discuss impact of low influenza vaccine rates on patients with cardiovascular disease
Cardiovascular disease (CVD) leads to one in four deaths in the United States, or nearly 800,000 deaths each year, according to the Centers for Disease Control and Prevention (CDC). To make matters worse, CVD coupled with an influenza virus infection substantially increases the risk of a serious or fatal cardiac event. Interestingly, influenza vaccination protects against cerebrovascular and cardiovascular events, according to studies.
People with heart conditions are particularly vulnerable to influenza-related heart complications. Yet, Americans with heart disease continue to have low influenza vaccination rates every year, according to a review study in the Journal of the American Heart Association by Khurram Nasir, MD, MPH, Jerold B. Katz Investigator and professor of cardiology at Houston Methodist. The influenza vaccination rate for American adults who are younger than 65 years of age and have CVD is less than 50%, compared to 80% in adults older than 65 with CVD. Influenza infection can lead to significant respiratory symptoms such as pneumonia, bronchitis and bacterial infection of the lungs. The virus' effects on the heart have historically been harder to dissect, in part because many patients already have a known predisposition to cardiac events. Furthermore, cardiac events often occur weeks after the disease onset.

Khurram Nasir, MD, MPH
Jerold B. Katz Investigator and Professor of Cardiology at Houston Methodist
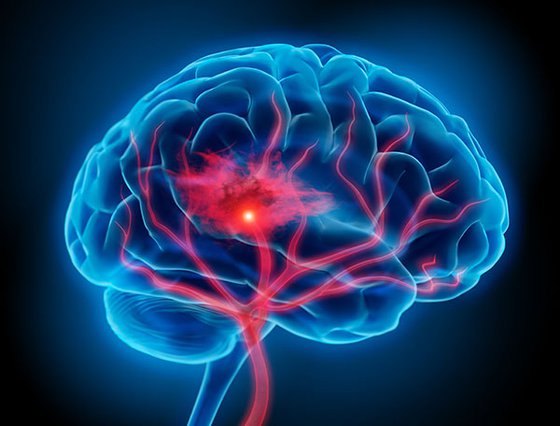
One in eight patients hospitalized with influenza experiences a cardiovascular event. Out of these patients, 31% require intensive care and 7% die because of the event. The effect of the influenza infection on the heart and vascular system is associated with the body's inflammatory response. This leads to blood clots, elevated blood pressure and swelling or scarring within the heart. The added stressors make atherosclerotic plaques within arteries more vulnerable to rupture, causing a blockage that impedes oxygen supply to the heart or brain and resulting in heart attacks and strokes. Thus, the effects on the cardiovascular system can be overwhelming to an already weakened heart muscle.

The rate of influenza vaccination in U.S. adults with CVD remains much lower than the national target despite known incidence of increased influenza-related complications, cardiovascular events, and deaths in this high-risk population. Vaccine uptake is a complex interplay of sociodemographic factors including age, insurance status, and health care access, as well as behavioral factors such as perception of vaccine efficacy and safety. Multi-level strategies to increase awareness of vaccine effectiveness and its limited side effect profile, and efforts to improve accessibility are urgently warranted, in this vulnerable and expansive patient population.

Khurram Nasir, MD, MPH
Jerold B. Katz Investigator and Professor of Cardiology at Houston Methodist
Additionally, non-cardiac complications from the viral infection, including pneumonia and respiratory failure, can worsen heart failure symptoms or heart arrhythmia. Studies have demonstrated that the vaccine is effective at protecting the general population and most vulnerable age groups (older than 65 and younger than 2) from severe cases of influenza. Furthermore, it's protective against cardiovascular mortality as well, especially among the high-risk population.
In his review study, Nasir and his team dove deeper into why the rates of influenza vaccine uptake were low within the population at high risk of CVD and found several sociodemographic factors. Influenza vaccine rates were particularly low in patients younger than 65 years of age, non-Hispanic black patients, those without health insurance and patients with lesser access to health care resources. Additionally, various psychological factors also played a role. These included perceived vaccine efficacy, vaccine safety, and sentiments towards vaccination.
According to Nasir, “The rate of influenza vaccination in U.S. adults with CVD remains much lower than the national target despite known incidence of increased influenza-related complications, cardiovascular events, and deaths in this high-risk population. Vaccine uptake is a complex interplay of sociodemographic factors including age, insurance status, and health care access, as well as behavioral factors such as perception of vaccine efficacy and safety. Multi-level strategies to increase awareness of vaccine effectiveness and its limited side effect profile, and efforts to improve accessibility are urgently warranted, in this vulnerable and expansive patient population.”
Because influenza viruses are constantly mutating, scientists alter the vaccine each year to match the likely prevalent strands. On average, a vaccine’s effectiveness at preventing infection is 40% — which is sufficient to significantly lower the risk of severe illness in most people. As a result of the demonstrated benefits conferred by influenza vaccination and the risks posed by this infection among those with CVD, several international scientific societies including the CDC, the American Heart Association and the European Society of Cardiology strongly recommend annual influenza vaccination in patients with CVD.
Unfortunately, many heart patients visit their cardiologists more frequently than their primary care providers, and cardiology practices typically do not provide flu vaccinations, though proposed recommendations may change in the future. Until then, it is incumbent upon both the cardiology provider and the primary care provider to communicate the increased risk to their patients and the importance of getting vaccinated. Clinicians and health care professionals should ensure high rates of influenza vaccination, especially in those with underlying chronic conditions, to protect against acute cardiovascular events associated with influenza.
Priyanka Bhugra, Gowtham R Grandhi, Reed Mszar, Priyanka Satish, Rahul Singh, Michael Blaha, Ron Blankstein, Salim S Virani, Miguel Cainzos-Achirica, Khurram Nasir. Determinants of Influenza Vaccine Uptake in Patients With Cardiovascular Disease and Strategies for Improvement. J Am Heart Assoc. 2021 Aug 3;10(15):e019671. doi: 10.1161/JAHA.120.019671.
Abanti Chattopadhyay, PhD, August 2022
Related Articles