


Clinical Research
Safe Refuse for N95s
System Quality & Patient Safety teams develop autoclaving protocol
After trying various masks and techniques and testing for fit, the team developed an autoclaving process for immediate-use
steam sterilization.
As more patients enter hospitals with COVID-19, focus has shifted to the dire shortage of N95s, the highly protective masks worn by health care workers to protect them from COVID-19 droplets while allowing safe respiration. While most of the attention focuses on supplying new masks, Houston Methodist’s System Quality & Patient Safety team is taking a different approach—with encouraging results.. Their new protocol, published online in Infection Control & Hospital Epidemiology by Cambridge University Press on April 17, 2020, entitled “Immediate-use steam sterilization sterilizes N95 masks without mask damage.”
Typically, infectious disease protocol requires an N95 to be discarded after one use. Based on that protocol, the COVID-19 crisis would require 3.5 billion N95 masks, while only 1% of that need can be met. Facing this reality, the Center for Disease Control now recommends saving and reusing N95 masks. Yet each attempt to safely don a contaminated N95 mask increases the risk of infection. In countries where equipment shortages have progressed, health care workers are being infected with COVID-19 at three times the rate of the general population, further reducing the hospitals’ ability to provide care.
To prevent the use of N95s beyond their capacity to be effective, Firas Zabaneh, MT, CIC, CIE, MBA, director of system infection prevention and control at Houston Methodist, and his team studied the problem. Based on their research, they found a way to reuse the precious masks without destroying their structural integrity—the very thing that makes them effective.
Zabaneh’s study focused on using an autoclave, a device for immediate-use steam sterilization (IUSS) to enable reuse of the now-precious N95 respirator masks. While hospitals often use autoclaves for sterilizing surgical and other equipment, they have not developed protocols for effectively reusing the masks—until now.
The challenge was to find an effective way to remove biological contamination from N95 masks without damaging their protective components or reducing their efficacy.

Firas Zabaneh, MT, CIC, CIE, MBA
Director, System Infection Prevention and Control
Professor, Cardiovascular Surgery
DeBakey Heart & Vascular Center
Houston Methodist
Specially constructed with protective components, N95 masks are made of thermoplastic elastomer straps, aluminum nose clip, polyurethane nose foam, polypropylene filter, and polyester shell and cover web made from thin fibers with an electrostatic charge. This design poses challenges for sanitization: Washing the masks with water decreased their performance by 21%, while alcohol reduced it by 37% and caused shrinkage. Ultraviolet irradiation compromised the masks integrity in 90% of cases, and bleach left residue that created additional risk for wearers.
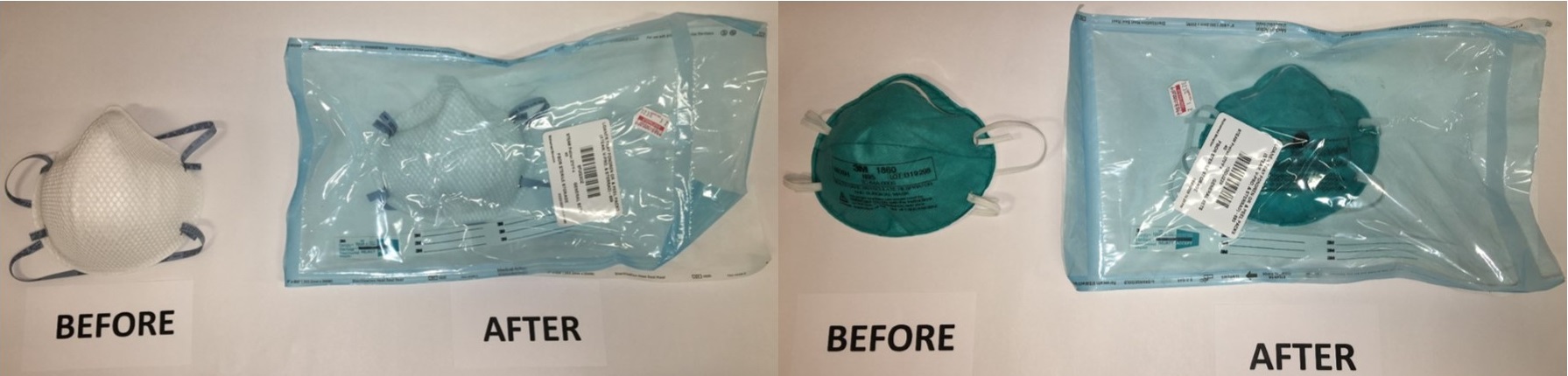
To develop the new IUSS protocol, Zabaneh and team photographed and fit-tested the N95s before the first IUSS test and for two additional IUSS cycles. Using a Steris Amsco Evolution HC1500 PreVac Steam Sterilizer autoclave to clean various styles of masks, packed in paper-plastic sterilization peel pouches, they identified two types of N95 masks that withstood quantitative fit testing, the gold standard for checking that N95s seal tightly to the wearer’s face to provide the promised 95% protection. The team also confirm that no biological or chemical contamination was present after each IUSS cycle.
Zabaneh’s research provides a promising option for wearing sterilized N95s while preventing the further spread of COVID-19 to health care workers. The next goal is to rapidly translate this finding to help the greater clinical community apply the new IUSS protocol to increase N95 reuse while decreasing COVID-19 contamination. Publication of the paper in Infection Control & Hospital Epidemiology will help other health care professionals gain access to the protocol.
References
1. U.S. Congress. Committee on Appropriations, Subcommittee on the Departments of Labor, Health and Human Services, Education, and Related Agencies. “Budget hearing on the Department of Health and Human Services.” (Date: 2/25/20). Text from: FDCH Political Transcripts. Available from: LexisNexis® Congressional; Accessed 3/24/20.
2. Strategies for Optimizing the Supply of N95 Respirators: COVID-19 [Internet]. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2020 [cited 2020Mar24]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/contingency-capacity-strategies.html
3. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. Published online February 24, 2020. doi:10.1001/jama.2020.2648
4. Viscusi DJ, King WP, Shaffer RE. Effect of decontamination on the filtration efficiency of two filtering facepiece respirator models. J Int Soc Respir Prot. 2007;24:93–107.
5. Martin SB, Mayor ES. 33. Electrostatic Respirator Filter Media: Filter Efficiency and Most Penetrating Particle Size Effects. Appl Occup Environ Hyg. 2000Aug;15(8):609–17.
6. Lindsley WG, Martin SB, Thewlis RE, Sarkisian K, Nwoko JO, Mead KR, et al. Effects of Ultraviolet Germicidal Irradiation (UVGI) on N95 Respirator Filtration Performance and Structural Integrity. Journal of Occupational and Environmental Hygiene. 2015;12(8):509–17.
7. Lindsley WG, Martin SB, Thewlis RE, Sarkisian K, Nwoko JO, Mead KR, et al. Evaluation of Five Decontamination Methods for Filtering Facepiece Respirators. The Annals of Occupational Hygiene. 2009 Apr;12(8):509–17.
LaVonne Carlson, August 2019








