restorative medicine
A New Age of Wound Care
Treating wounds with telomerase mRNA in a lipid nanoparticle counteracts telomere shortening to improve wound healing.
Treating wounds with telomerase mRNA in a lipid nanoparticle counteracts telomere shortening to improve wound healing.
Despite our best efforts, aging happens to us all.
While our entire bodies exhibit markers of this infernal process, its impact on the skin is especially evident. In addition to compromised skin integrity and functionality, regenerative potential is also impaired. Even more consequential, senescent skin cells—those that are aging and no longer divide—secrete more proinflammatory cytokines and produce more reactive oxygen species, which severely compromises wound healing.
Cellular aging and the resulting impairments are caused in part by telomere erosion. Telomeres are protective caps at the end of chromosomes that prevent damage and fraying. Comprised of a repetitive DNA sequence bound by special proteins, telomeres are common in eukaryotes and required for cell division in most organisms. They do a great job, but with each cell division, telomeres shorten, until, eventually, they become too short for the cell to divide, and the cell dies.
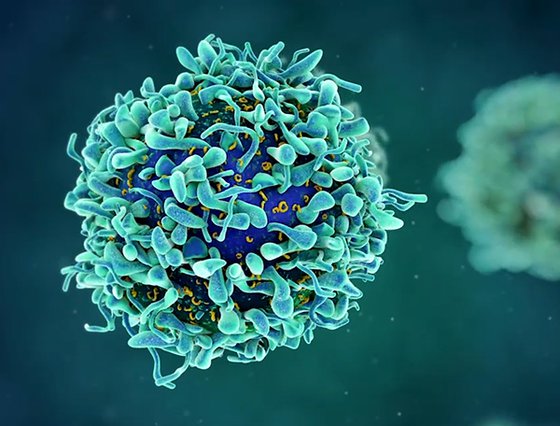
Telomerase is an enzyme made up of a catalytic protein subunit—human telomere reverse transcriptase (hTERT)—and a non-coding RNA component (hTR) that counteracts telomere shortening by adding telomere repeat sequences to the ends of chromosomes. Unfortunately, it is only expressed in certain cell types, such as stem cells and cells that are proliferating.
The objective was to study the impact of a novel hTERT mRNA therapeutic on skin regeneration. Our results are promising and indicate that point-of-care treatment with an mRNA nanotherapeutic can increase telomerase activity in human skin cells.
John Cooke, MD, PhD
Joseph C. “Rusty” Walter and Carole Walter Looke Presidential Distinguished Chair in Cardiovascular Disease Research
Evidence suggests that telomerase-expressing cells are resistant to telomere dysfunction and can promote wound healing. In fact, hTERT plays a role in genomic DNA damage repair and protection against oxidative stress. In a study published earlier this year, co-corresponding authors John Cooke, MD, PhD, Joseph C. “Rusty” Walter and Carole Walter Looke Presidential Distinguished Chair in Cardiovascular Disease Research, and Biana Godin, MScPharm, PhD, Associate Professor of Nanomedicine, demonstrated that telomerase mRNA lipid nanoparticles (LNP) can enhance human skin engraftment for wound healing.
Traumatic skin wounds are a significant global public health burden. Annually, burn injuries affect 11 million people with more than 300,000 deaths. Deep burns and severe chronic wounds are complex and early surgical interventions such as wound excision and immediate skin grafting significantly increase healing and patient survival. Currently, autologous split-thickness skin grafts (STSG) are the standard-of-care for deep partial-thickness and full-thickness burns, though complications include pain, scarring, pruritis, infection, delayed healing and donor site morbidity.
Previously, this Houston Methodist group showed that in aged human cells, the introduction of hTERT mRNA enabled transient expression of hTERT, which restored telomere length, cell replicative capacity, cell morphology and functions, and reduced DNA damage markers. The biggest limitation of their novel approach was the instability of mRNA in liquids, so in their most recent work, they used lipid nanoparticles to overcome the mRNA instability. Their results show enhanced performance of human skin cell suspension (hSCS) in wound healing using a human telomerase reverse transcriptase mRNA carried by a lipid nanoparticle.
Artist rendering of encapsulation of mRNA into a lipid nanoparticle
The team evaluated hTERT mRNA LNP-based therapy for enhancing engraftment of hSCS using a partial-thickness wound healing model.
“The objective was to study the impact of a novel hTERT mRNA therapeutic on skin regeneration, “said Cooke. Our results are promising and indicate that point-of-care treatment with an mRNA nanotherapeutic can increase telomerase activity in human skin cells.”
Godin added, “This effect is associated with an increase in human cells in the wound bed and upregulation of the cellular proliferation marker Ki67. We also experienced a reduction in the senescence marker p21 and DNA damage marker 53BP1, which indicates that mRNA telomerase may be useful in improving cell viability and augmenting wound healing.”
This study demonstrates the promise of telomerase therapy to enhance engraftment and proliferative capacity and mitigate DNA damage of hSCS in a partial-thickness humanized wound model. To fully realize the potential of this strategy, further development is needed in the context of wound healing. “These results establish proof-of-concept of point-of-care methodology that could be extended to other RNA-based cell therapies,” Cooke said.
David F. Chang, Karem A. Court, Rhonda Holgate, Elizabeth A. Davis, Katie A. Bush, Andrew P. Quick, Aldona J. Spiegel, Maham Rahimi, John P. Cooke, and Biana Godin
Heather Lander, PhD
December 2024
Related Articles